Translate this page into:
Primary extradural hydatid cyst extended to paraspinal muscles
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Primary spinal epidural hydatid cyst without bony involvement is extremely rare. Authors report the case of a 44-year-old female brought to their attention for a rapidly progressive paraplegia. Magnetic resonance imaging (MRI) revealed extradural multiple cysts with “bunch of grapes” appearance extended to the paraspinal muscles through neural foramina without bony involvement on computed tomography (CT) scan. Histopathologic examination after a surgical approach confirmed the diagnosis of hydatid cyst. The early postoperative period showed a progressive improvement of her neurological deficit. The long-term follow-up under discontinued antihelminthic chemotherapy was uneventful.
Keywords
Extradural
hydatid cyst
intraspinal
magnetic resonance imaging
paraspinal muscle
Introduction
Hydatid disease remains an important health issue in livestock of developing countries where veterinary control is infrequent.[12] This is a zoonosis caused by Echinococcus granulosus. Its definitive hosts are usually dogs and occasionally cats, wolves, and foxes.[3] Livestock represents the intermediate host.[1–3] Human being contracts the disease from direct contact with the infected animal or its feces or via contaminated food.[14] Hydatid disease of spine occurs in 1% of hydatidosis and is mostly extended from pulmonary infestation and less often begins primarily in the vertebral body.[4] Primary extradural hydatid cyst is exceptional with few reported cases.[4] Moreover, muscles are regarded to be unsuitable for parasite survival.[5] We report a particular case of primary extradural hydatid cyst extended to paraspinal muscles through a foramina revealed by a spinal cord compression syndrome. Our biggest challenge after the diagnosis was the surgical management in so far these hydatid cysts should be removed without rupturing them. Spontaneous or surgical rupture might lead to catastrophic dissemination. En bloc resection without inducing rupture and spreading the daughter cysts is the recommended treatment strategy and accepted to be curative for muscular and extradural hydatid cyst.[45]
Case Report
A previously healthy 44-year-old female was admitted in our department with spinal cord compression syndrome. She was a dog owner and came from a rural area. Her complaints started 20 days before with diffuse back pains followed by a rapidly progressive weakness and numbness in both legs resulting in walking difficulty. This condition was complicated 3 days before her admission by complete paraplegia with sphincter dysfunction. Neurological examination revealed a flaccid paraplegia with 0/5 bilateral muscle strength with hypoesthesia below T10. Superficial abdominal reflexes, and ankle and knee jerks were absent with indifferent plantar response.
Lumbar computed tomography (CT) scan revealed no vertebral lesions [Figure 1a]. Magnetic resonance images (MRI) of the spine demonstrated multiple well-defined extradural cystic lesions with a “bunch of grape” appearance that extended from T11 to L4. These lesions were hypointense on T1-weighted images and hyperintense on T2-weighted images with an extension to the right paraspinal muscle through L1 neural foramina. Paraspinal lesions were surrounded by a single wall which was hyperintense on T2-weighted images, resulting in a multilocular mass of 2.5 × 6 cm [Figure 1b and c]. The spinal cord and the cauda equina were severely compressed. Thoracic and abdominal CT scan was normal and hydatid serology was negative.
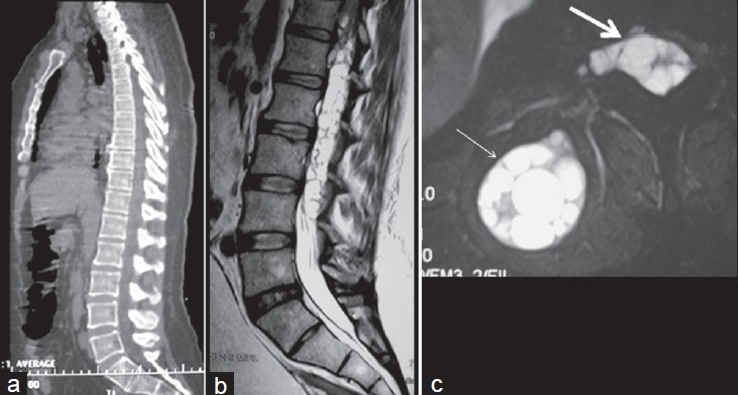
- Preoperative imaging: (a) sagittal CT scan of the spine did not show any abnormality of the vertebrae; (b) sagittal T2-weighted MRI of the lumbar spine revealing compression of spinal cord and dural sheath by hydatid cysts; (c) axial T2-weighted MRI of the lumbar spine showing intraspinal hydatid cysts (white thick arrow) and their muscular extension (white slender arrow)
Intraspinal cysts were removed through an L1 to L4 laminectomy. Then, the same skin incision was used to perform right paraspinal muscle dissection allowing “en bloc” resection of the muscular encapsulated cysts and their foraminal extensions [Figure 2]. Operative fields were soaked with hydrogen peroxide and hypertonic saline (20%).

- Intraoperative imaging: (a) muscular encapsulated hydatid cysts (white arrow); (b) intraspinal hydatid cysts after laminectomy (white arrow); (c) en bloc resection of the muscular hydatid cyst; (d) the capsule was filled with hydatid cysts on its opening; (e) hydatid cysts
Parasitological examination found sterile cysts without hydatic scolex and the diagnosis of hydatid cyst was confirmed on histopathologic examination.
Albendazole treatment was initiated in the early postoperative stage: 400 mg twice a day during a month with 15-day free-drug intervals. Patient's symptoms were relieved progressively after surgery. No recurrence has been found over 1-year follow-up [Figure 3].

- Postoperative imaging. Sagittal T2-weighted MRI of the lumbar spine did not show any hydatid cyst
Discussion
Hydatid disease of spine was first described by Churrier in 1807 and accounts for less than 1% of all cases of hydatid disease.[4–6] However, extradural hydatid cyst without vertebral involvement is very rare even in endemic areas.[14] Human being is infected by ingesting the eggs of E. granulosus. The chitinous coat of the eggs is dissolved and the liberated embryos pass through the intestinal mucosa into the portal venous system and reach different organs via the blood stream.[6] Within 3 weeks, the embryos develop into larvae and start producing cysts.[6] While traversing the major filters of the body represented by liver and lung, 75% and 15% of the larvae will be trapped, respectively.[14] According to Sener et al., another atypical journey might explain the primarily epidural location of the parasite.[7] They advocate that the parasite penetrates the intestinal muscle and directly enters into the inferior vena cava system through small venous connections between this system and portal circulation. Then, the parasite reaches the retroperitoneum, spinal and paraspinal structures via lumbar epidural venous plexuses.[89] This last mechanism can explain the epidural location of hydatid cysts in our patient. Moreover, the development of hydatid cyst in paraspinal muscles is uncommon in so far the high lactic acid level of muscle is proned to be unsuitable for the parasite survival and muscular contractions prevent fixation of larva to the tissue.[7] Although in our patient the paraspinal hydatid cyst would have probably resulted from extradural extension, this remains a very rare condition. The clinical presentation is constituted by progressive cauda equina or spinal cord compression syndrome according to the location of the disease, but there is no pathognomonic symptom.[48] Thus, physicians must be aware of this diagnosis in patients from endemics regions or with a positive history of hydatid disease. MRI represents the gold standard for diagnosing spinal hydatid cyst.[47] On MRI, hydatid cysts appear as well-circumscribed, cystic lesions, with CSF-like signal intensities.[6] The cyst wall is usually thin and regular with no septations. The cysts are hypointense on T1-weighted images. On T2-weighted images, they appear hyperintense with sharply defined, hypointense cyst wall which shows mild enhancement following intravenous gadolinium, reflecting the vascularity of the pericyst in case of muscle hydatid cyst.[37] But there is no contrast enhancement either in extradural or intradural hydatid cysts.[6] Extradural spread of hydatid cysts through widened neural foramina into muscles may result in a “bunch of grapes” appearance.[78] CT scanning may be more convenient in vertebral bone lesions’ diagnosis. In our case, the CT scan of the spine revealed no vertebral involvement. Surgery remains the treatment of choice in extradural hydatid cyst and consists of decompressive laminectomy and cyst removal. En bloc resection is required in muscle hydatid cyst to reduce the seeding of the parasite. Scolicidal agent such as hydrogen peroxide and hypertonic saline 20% might decrease the parasite dissemination, and therefore should be used to soak the operative field like in our case.[6] A discontinued postoperative antihelminthic chemotherapy might reduce the recurrence rate, which is about 30–40%.[10]
Conclusion
Primary spinal epidural hydatid cyst should be considered in the differential diagnosis of spinal cord compression syndrome. The treatment requires surgical decompression. Moreover, the using of scolicidal agents (hypertonic saline, hydrogen peroxide) during surgical procedure and adjuvant chemotherapy based on antihelminthic agents such as albendazol or mebendazol reduces dramatically the recurrence rate. However, the incidence of this disease can be reduced by conducting preventive programs against E. granulosus, including deworming of dogs, elimination of stray dogs, and practicing personal hygiene (hand washing). These programs might be led by the physicians who practice medicine in rural areas.
Source of Support: Nil
Conflict of Interest: None declared
References
- Magnetic resonance imaging and computerised tomography findings in an intraspinal extradural hydatid cyst mimicking tuberculous spondylitis: A case report. Cases J. 2009;2:7109.
- [Google Scholar]
- Primary cervical paraspinal hydatid cyst: A case report. J Neurol Sci [Turk]. 2011;28:97-100.
- [Google Scholar]
- Primary spinal epidural hydatid cyst with intrathoracic extension. Neurosciences (Riyadh). 2009;14:81-3.
- [Google Scholar]
- Long-term result of treatment for paraspinal and extradural hydatid cyst: A case report. Acta Orthop Traumatol Turc. 2009;43:267-71.
- [Google Scholar]
- Primary spinal extradural hydatid cyst causing spinal cord compression. Indian J Orthop. 2007;41:76-8.
- [Google Scholar]
- Primary paraspinal hydatid cyst treated with puncture, aspiration, injection and re-aspiration (PAIR) technique: A case report. Eur Spine J. 2009;18:165-7.
- [Google Scholar]
- Primary spicnal epidural hydatid cyst: A case report. Pan Arab J Neurosurg. 2001;5:50-2.
- [Google Scholar]






