Translate this page into:
Endoscopic endonasal trans-sphenoid surgery of pituitary adenoma
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
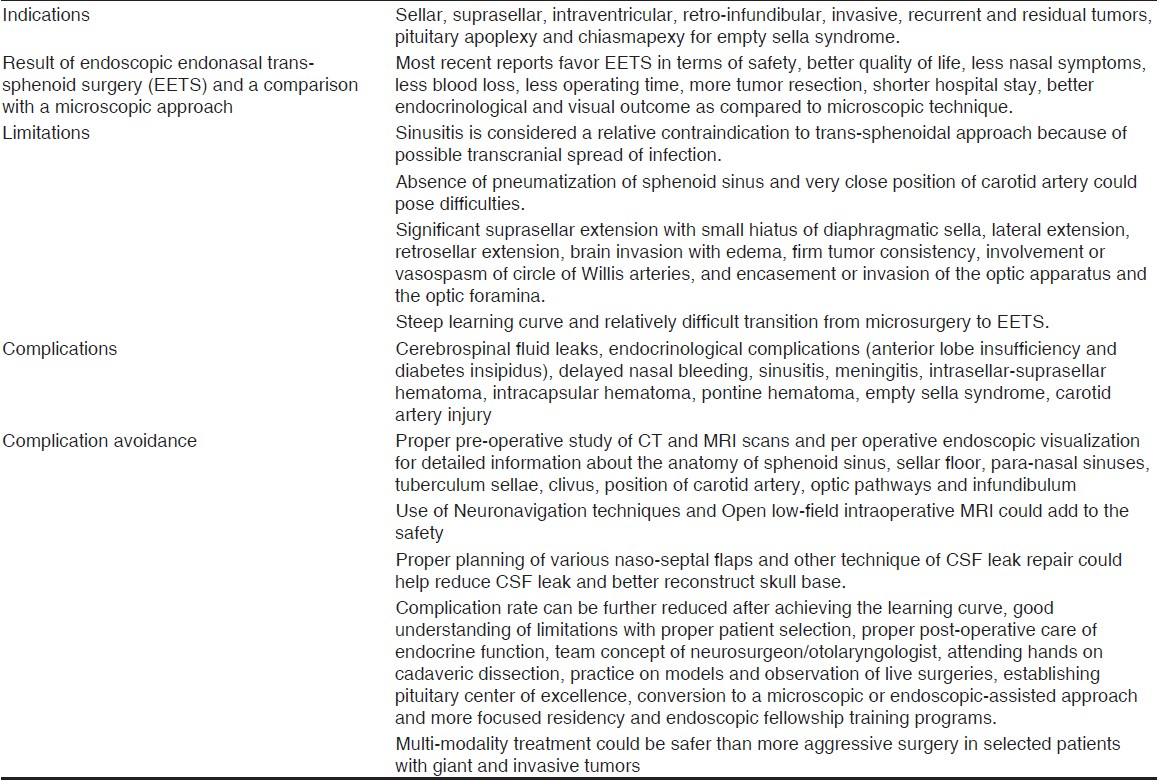
Endoscopic endonasal trans-sphenoid surgery (EETS) is increasingly used for pituitary lesions. Pre-operative CT and MRI scans and peroperative endoscopic visualization can provide useful anatomical information. EETS is indicated in sellar, suprasellar, intraventricular, retro-infundibular, and invasive tumors. Recurrent and residual lesions, pituitary apoplexy and empty sella syndrome can be managed by EETS. Modern neuronavigation techniques, ultrasonic aspirators, ultrasonic bone curette can add to the safety. The binostril approach provides a wider working area. High definition camera is much superior to three-chip camera. Most of the recent reports favor EETS in terms of safety, quality of life and tumor resection, hospital stay, better endocrinological, and visual outcome as compared to the microscopic technique. Nasal symptoms, blood loss, operating time are less in EETS. Various naso-septal flaps and other techniques of CSF leak repair could help reduce complications. Complications can be further reduced after achieving the learning curve, good understanding of limitations with proper patient selection. Use of neuronavigation, proper post-operative care of endocrine function, establishing pituitary center of excellence and more focused residency and endoscopic fellowship training could improve results. The faster and safe transition from microscopic to EETS can be done by the team concept of neurosurgeon/otolaryngologist, attending hands on cadaveric dissection, practice on models, and observation of live surgeries. Conversion to a microscopic or endoscopic-assisted approach may be required in selected patients. Multi-modality treatment could be required in giant and invasive tumors. EETS appears to be a better surgical option in most pituitary adenoma.
Keywords
Neuroendoscopy
nasal cavity surgery
pituitary neoplasm
pituitary adenoma
sphenoid sinus
sphenoid bone surgery
Introduction
Neuroendoscopy has grown rapidly in the last 25 years as a therapeutic modality for treating a variety of brain and spinal disorders.[1–3] Endoscopic endonasal trans-sphenoid surgery (EETS) is gaining wide acceptance as the first-line treatment of most pituitary adenomas. This article is aimed to review endoscopic Tran's sphenoid management of pituitary tumor. This review is based on 15 years search on this subject on PubMed, Google, and Medline plus.
Investigations
Detailed pre-operative study of CT and MRI scans,[4] per-operative endoscopic visualization,[5] and pre-operative three-dimensional modeling of the pituitary adenoma[6] can provide information about the anatomy of sphenoid sinus, sellar floor, para-nasal sinuses, tuberculum sellae, clivus, position of carotid artery, optic pathways, and infundibulum. A detailed study of lesion and its surrounding structures is important to improve the safety and accuracy of surgery. Although endonasal anatomical variations are frequent, they do not pose a relevant obstacle in the EETS technique.[7]
Pre-operative thorough examination of endocrinological status, visual field, and visual acuity is also essential. Diffusion tensor imaging assessments with fractional anisotropy and mean diffusivity values may help to estimate the response of visual improvement after surgical therapy in the early post-operative period.[8]
Technique
This procedure utilizes a zero or 30 degree endoscope (usually 4 mm wide and 18 cm long). Thirty centimeter long telescope has an advantage over 18 cm scope. It keeps camera away from nasal opening which allows easy manipulations of instruments. General anesthesia is administered and the nasal mucosa of the middle turbinate is injected with a 1:100,000 epinephrine solution to induce vasoconstriction. The epinephrine solution soaked in cotton is also used to induce vasoconstriction of the whole nasal cavity mucosa. Thorough inspection of both the nasal cavities is done to identify normal structure and any anatomical variation. The middle turbinate can be resected or lateralized depending on the type of pathology. It is better to resects turbinate in large lesion to get more space for dissection. This turbinate can be used for sellar reconstruction. In patients with concha bullosa, conchal bone can be removed which can be used for sellar reconstruction after EETS surgery.[9]
Sphenoid ostium is identified which lies usually 1-1.5 cm superior to the choana. A naso-septal flap is raised if needed.[10] The pedicled naso-septal flap may not be sufficient in large dural defect especially in children less than 14 years of age.[11] Bilateral naso-septal flaps could be required in these cases.[12] The naso-septal flap must be raised at the beginning of the operation to protect the posterior pedicle during the expanded approach. In most pituitary tumor cases, an intraoperative cerebrospinal fluid leak is not expected but may be encountered. In these cases, a “rescue” flap approach can be used.[13] In 1999, Dr. Gustavo Hadad and Dr. Luis Bassagaisteguy, from Argentina, developed a flap based on sphenopalatine artery, the vessel with the largest possible vascular territory in the nose. The sphenopalatine artery is the terminal branch of the internal maxillary artery, and it enters the nose through the sphenopalatine foramen. At the foramen, it then divides into two branches. The posterior branch (septal artery) runs over the rim of the posterior choana on the sphenoid in the sub-mucosal plane. This fact allows the flap to be harvested from the nasal septum in a sub-perichondrial and sub-periosteal fashion. The anterior limit is at the entrance of the nostril. It should be designed as long as possible. Posteriorly, incision follows the posterior border of the nasal septum and then arches over the choana. Part of the superior nasal septal mucosa is left to preserve olfaction.
Endoscope is positioned superiorly at 12 o’clock in right nostril to optimize the available space. Suction is usually entered into the 6-o’clock position in the right nose and dissecting instruments can be introduced through the left nostril. Sphenoid ostium is enlarged with Kerrison rongeurs. Sphenoid rostrum and posterior vomer is removed to open the whole anterior wall of the sphenoid sinus. This creates the desired single rectangular cavity and allows identification of key anatomical landmarks. The medial optico-carotid recess (OCR), carotid protuberance, the sellar face, clival recess and the strut of bone over the superior inter-cavernous sinus (SIS) should be recognized. The medial OCR represents the ventral surface of the medial clinoid and is the key anatomical landmark in this region. An entry at the level of the medial OCR allows simultaneous access to the carotid canal, optic canal, sella turcica, and medial cavernous sinus. It is analogous to a “key hole” during a conventional pterional craniotomy. The medial OCR does not need to be opened for the removal of pituitary tumors unless there is significant suprasellar and lateral extension toward the optico-carotid cistern. The sphenoidotomy is widened to include the lateral recess of the sphenoid extending lateral to the carotid canal especially for the expanded approach. The exposure is then extended rostrally to expose the posterior cells of the ethmoid sinus and the planum–tuberculum junction. Finally, the floor of the sphenoid is resected back to the level of the clivus. This is particularly important in the case of macroadenomas with significant suprasellar extension. By reducing the floor of the sphenoid, a greater caudal-to-rostral trajectory into the suprasellar space is created. Any intrasphenoidal septations must be removed with care, because the paramedian septations often lead to the internal carotid artery. The sphenoid sinus mucosa is removed and the venous bleeding is controlled by irrigation with warm saline. Wide opening of sella is better for removal of large tumor. Removal of the bone overlying the SIS is imperative for lesions extending into the anterior cranial fossa. Bone removal over the sellar face should extend laterally over the medial portions of each cavernous sinus and rostro-caudally to expose both the superior and inferior inter-cavernous sinus. Surgeons who are beginner in endoscopy may fail to undertake an adequate exposure sometimes. This eliminates the primary advantage of endoscopic surgery of delivering divergent focal light and magnification which facilitates superior visualization and dissection. Combination of micro-curettes and micro dissectors are used to remove tumor within and above the sella. Endoscopic tumor resection uses techniques identical to those of microsurgery (internal debulking, capsular mobilization, and extracapsular dissection of neurovascular structures, along with coagulation and capsule removal).
Cerebrospinal fluid (CSF) leak if encountered can be repaired with fibrin glue, fat, and fascia lata and vascularized nasoseptal flap. CSF diversion techniques have been reported to manage CSF leak. A simple purely synthetic repair of low-grade CSF leaks with a hydrogel sealant is described.[14] Another simple and quick technique involving layered fibrin glue and gelatin sponge is also effective.[15] More complex defects after pituitary surgery should be repaired with button graft technique.[16] Multilayer technique, using autologous materials such as fat, fascia lata, bone, and mucoperiosteum, is frequently used for large defect.[1718] In recent cases, dural opening has been sutured.[19] The trans-septal approach preserves the total septum which can be used for future reconstructions.[20]
The bilateral endonasal approach provides a wide working area as compared to single nostril approach.[2122] After anterior sphenoidotomy, the endoscope can be fixed or can be held by the assistant in one nostril and the instruments can be inserted through any of the nostril. The bilateral endonasal approach provides a wide working area without the need for special instruments. Mucosal dissection can be modified (unilateral or bilateral dissection) depending upon tumor extension. This approach is better suitable for more extensive tumors. Binostril approach is strongly advocated especially for all expanded endoscopic approaches. Special transnasal trans-sphenoidal speculums with interchangeable blades and unique blade angulations were found to be safe. It allows optimal exposure and can be used interchangeably with microscopic or endoscopic techniques.[23]
Traditional boundaries of the trans-sphenoidal approach can be extended in antero-posterior and lateral planes.[24–26] The evolution of the endoscopic endonasal trans-sphenoidal technique, which was initially reserved only for sellar lesions, has lead to a progressive possibility to access the skull base from the nose. This route allows midline access and visibility to the suprasellar, retrosellar and parasellar space without brain retraction. This technique allows us to treat a variety of suprasellar and parasellar lesions which were traditionally approached by trans-cranially. Detailed knowledge of anatomy is must to properly perform this technique and to avoid complications. CSF leak remains a challenge and proper cranial base reconstruction and sealing of the leak is important. Such extended endoscopic approaches require an advanced and specialized training. Endoscopic endonasal transposition of the pituitary gland and its stalk can provide a valuable corridor to the retroinfundibular region with preservation of pituitary function.[27] The interpeduncular cistern, including the retroinfundibular area, is one of the most challenging regions to approach trans-nasally. The pituitary gland and the infundibulum guard the region when an endonasal route is undertaken. Superior transposition of the pituitary gland and infundibulum can be performed to access this complex region. Preservation of normal pituitary function can be achieved in over 85% cases but remains a concern in this technique. This approach should only be pursued once significant experience with endoscopic endonasal approaches has been acquired.
The capsule of the tumor is the compressed normal pituitary gland. The normal adenohypophysis was more often found at histopathology in the extracapsular excisions, rather than in the intracapsular excisions. The trans-sphenoidal pseudocapsule-based extracapsular resection approach provides a more effective and safe alternative compared to the traditional intracapsular technique.[28] Better tumor removal, good remission and lower recurrence rate could be achieved compared to intracapsular approach. Gross total extracapsular dissection may be accomplished either by using a standard approach to the pituitary fossa or by extending the exposure. This technique could need removal of a portion of the planum sphenoidale and division of the superior inter cavernous sinus especially in tumors with suprasellar extension. Separation of the tumor from the normal gland, stalk, and cavernous sinus contents could be possible. It should be noted that the improved visualization provided by the endoscope does allow extracapsular dissection in many cases but it is not always possible especially in giant tumor. Intracapsular resection has also been found to be a safe and effective treatment.[29]
One has to pay proper attention to anatomical considerations for endoscopic endonasal skull base surgery in pediatric patients.[30] Various Neuronavigation techniques can make reoperation easier, faster, and safer.[31–37] Open low-fields intraoperative MRI, using contrast-soaked cottonoid packing in the tumor resection cavity, can be used to monitor the precise extent of tumor removal.[38] Integrating MR angiography into surgical neuronavigation provides superior visualization of the carotid arteries.[39]
Soft-tissue removal is often a rate-limiting aspect in endoscopic procedures, especially when the tissue is dense or fibrous. Ultrasonic aspiration[40] and other instruments can be used to remove tissue, without generating heat, through the working channel of the endoscope.[41] The side-cutting tissue resector is also safe, easy to use, and effective tool for non vascularized firm tumors.[42] The ultrasonic bone curette is a useful tool for bone removal.[43] The pulsed laser-induced liquid jet system can achieve safe and optimum removal without vascular damage.[44]
An endoscope holder can be useful when another expert endoscopic surgeon is not available to assist. This allows both hands to be free.[45] The management of intradural bleeding can be done with the use of a thrombin-gelatin haemostatic matrix.[46] A high definition (HD) camera is much superior to standard three-chip camera. Improved resolution, color information, and larger viewing field are some of the advantages of HD.[47] Three-dimensional endoscopic trans-sphenoidal pituitary surgery with improved depth perception[48] and Video endoscopic endonasal pituitary surgery could prove to be an excellent method in coming years.[49]
Hypothalamic-pituitary-adrenal function is usually preserved in non-functioning pituitary macroadenoma. Peri-operative steroid treatment should be given only in patients with hypocortisolism.[50]
Indications
Endoscopic endonasal trans-sphenoidal surgery is indicated in sellar[51] and suprasellar tumors.[2526] Staged[52] or combined endoscopic trans-sphenoidal-transventricular approach[253–55] for resection of a giant pituitary adenoma with ventricular extension can achieve a gross total removal. Endoscopic endonasal transposition of the pituitary gland and its stalk can provide a valuable corridor to the retroinfundibular tumor.[27] Pituitary tumors with invasion in the internal carotid artery and cavernous sinus could be managed by EETS.[5657] Recurrent and residual tumor,[58] and patients with pituitary apoplexy[5960] could be treated by EETS. Chiasmapexy for empty sella syndrome with post-operative visual deterioration[61] can be effectively performed by EETS [Table 1].
Result of Endoscopic Endonasal Trans-Sphenoid Surgery and Comparison with Microscopic Approach
Endoscopic intracranial surgeries are increasingly used in various conditions.[62–64] Endoscopic surgery is a better technique in removal of a suprasellar tumor than the microscopic approach due to the better visualization.[65] The avoidance of craniotomy, brain retraction, and reduced neurovascular manipulation with less morbidity are potential advantages.[66] Endoscopic pituitary surgery was found to be safe.[5167–69] The quality life was better in terms of patient discomfort and pain perception[70–73] as compared to conventional microscopic technique. Operating time,[7174–77] hospital stay,[71727476–78] and blood loss[72–7477] was less in the endoscopic technique as compared to the microscopic technique.
Nasal symptoms
The nasal outcome was better in the endoscopic group as compared to microscopic group. Post-operative nasal packing is not necessary and post-operative discomfort is minimal.[777980] On the other hand, the overall nasal symptoms did not show any significant change in the earlier study.[81]
Tumor resection
Amount of tumor resection was better in the endoscopic technique compared to microscopic technique.[7375–7882–87] In other study, the extent of tumor resection was same in the endoscopic and microsurgery technique.[71]
Visual outcome
Ophthalmological recovery was better in the endoscopic group as compared to the microscopic group.[87] On the other hand, the visual outcomes of microscopic and endoscopic techniques were the same.[7688]
Endocrinological outcome
The endocrinological outcome of endoscopic technique was superior to traditional microsurgical technique.[7376778485878990] In one earlier study, similar results were observed in both the techniques.[71]
Non functional pituitary tumors
The amount of tumor resections, endocrinological outcome of anterior pituitary function and ophthalmological recovery were significantly better in endoscopic group as compared to microscopic group. There was no significant difference in morbidity in two groups.[87]
Functional tumor
Controls of tumor growth and endocrinopathy was better and complications were less in EETS as compared to other treatment modalities.[91]
Growth hormone secreting tumors
A majority of the EETS series reported a high rate of gross-total tumor resection and endocrinological remission in acromegaly patients.[8485] Factors affecting the success of the endoscopic surgery were lesion size, suprasellar/parasellar extension, and the degree of sella floor erosion.[92] Trans-sphenoidal surgery in longstanding acromegaly frequently poses greater challenges than other tumors.[93] On the other hand, similar clinical outcome was reported after EETS and the microsurgical technique in growth hormone secreting tumor.[94]
Cushing disease
Trans-sphenoidal pituitary surgery is the primary therapy for Cushing disease because of its potential to produce lasting remission without the need for long-term drug or hormone replacement therapy. It is also safe.[95–99] The EETS led to shorter anesthesia time, less blood loss, and shorter hospital stay compared to the sub-labial trans-septal approach. On the other hand, there was no difference between the two surgical procedures with respect to cure or complications in other study.[100]
Thyroid-stimulating hormone secreting pituitary tumor
The diagnosis of thyroid stimulating hormone secreting pituitary lesions is often delayed. The clinical picture is heterogeneous and it is difficult to treat. A trans-sphenoid approach can effectively treat such cases.[101]
Prolactinoma
Most of the prolactinomas now can be managed by medical therapy. Medical therapy-resistant prolactinomas need surgery. Endoscopic techniques are found to be better than the microscopic technique. The advantages of extended endonasal approaches are most profound in tumors with suprasellar extension and cavernous sinus invasion.[969899] Endoscopic trans-sphenoidal surgery offers better removal of the adenoma from the medial cavernous sinus wall as compared to transcranial surgery. Gamma Knife surgery and medical therapy should be supplementary treatment options after endoscopic trans-sphenoidal surgery especially with gross cavernous sinus involvement lateral to carotid artery.[102]
Limitations
Sinusitis is considered a contraindication to trans-sphenoidal approach because of possible transcranial spread of infection. Now there are reports of the concurrent trans-sphenoidal approach and endoscopic sinus surgery in selected patients with chronic rhinosinusitis and pituitary adenoma.[103] The absence of pneumatization of sphenoid sinus and very close position of carotid artery could pose difficulties in EETS.
Significant suprasellar extensions with small hiatus of diaphragmatic sella, lateral extension, retrosellar extension, brain invasion with edema are some of the limitations of EETS. Firm tumor consistency, involvement or vasospasms of the circle of Willis arteries, and encasement or invasion of the optic apparatus are also some of the limitations of endoscopic trans-sphenoid surgery. Presence of these findings increases risk of trans-sphenoid surgery even in the expert hands. Open craniotomy as the initial operation should be performed in such cases.[104] Although significant suprasellar extensions, lesions with intraventricular spread and retro-infundibular lesions can be managed by the endoscopic approach after gaining sufficient experience, it carries more complications in the initial learning curve.
Learning curve
EETS like every other surgical technique do have a learning curve. Results are poor in the beginning of the learning curve. This also explains why complications were higher in some endoscopic series as compared to other series. These complications are significantly reduced after achieving this learning curve which could vary between 17 surgeries in O’Malley et al. series and 50 surgeries in Leach et al. series.[105106] Attending workshops, hands on cadaveric dissection, practice on models, and observation of live surgeries can reduce the learning curve. A training model using a skull and eggs is useful to improve surgical techniques in EETS.[107]
Transition from microsurgery to endoscopic trans-sphenoidal pituitary neurosurgery
Transition from microsurgery to EETS requires steep learning curve. The collaboration between otolaryngologists and neurosurgeons, attending live workshops, hands on cadaveric dissection, training on models and a controlled, supervised residency training programs could improve the learning curve.[108]
Complications and its Avoidance
Complication rates were low in most endoscopy group as compared to the microscopic technique.[71757691] On the other hand, comparable complications were reported in both the groups.[78] Gondim et al. observed 26.9% complications in their series. Post-operative CSF leaks, delayed nasal bleeding, sphenoid sinusitis, carotid artery injury, and meningitis occurred in 2.6%, 1.9%, 1.6%, 0.9%, and 0.6%, respectively. Endocrinological complications were observed in 17.9% cases out of which anterior lobe insufficiency was seen in 11.6% and diabetes insipidus in 6.3% cases.[109] Empty sella syndrome, diabetes insipidus, CSF rhinorrhea, post-operative intracapsular hematoma were also reported in other studies.[1761110–115]
CSF leak
Intraoperative CSF leaks were classified as grade zero when there was no intraoperative CSF leak. Grades 1 and 2 were classified based on the degree of CSF leakage (low or high output) and size of the opening in the arachnoid membrane (<5 or ≥5 mm).[116] A higher incidence of post-operative CSF leak was noted in the endoscopic approach as compared to the microscopic technique.[737789] The higher incidence of complication in the endoscopic group could be due to large lesions with higher proportions of suprasellar tumors and also due to initial learning curve in the endoscopy group. On the other hand, low CSF leak was also reported in the endoscopic group.[117] CSF leak can be prevented or reduced by the multi-layered repair and the dural suture technique with a fascia lata graft.[14–19118]
Nasal complications
Nasal complications occurred in 29.6% of the operated cases. The most common complications were prolonged nasal crusting (10.4%), synechia formation (8.8%), and septal deviation (3.7%).[119] Rhinosinusitis/mucocele occurs in about 6% cases.[120121] The most frequent sinusitis complication was sphenoiditis followed by ethmoid sinusitis and maxillary sinusitis.[121]
Visual deterioration
Visual deterioration though rare could be seen in cases requiring more dissection to the under surface of optic apparatus such as in giant invasive pituitary tumor and craniopharyngioma.[122]
Olfactory changes
Although the transnasal endoscopic approach to the sella removes structures known to contribute to olfactory function, it has no clinically significant effect on olfaction.[123]
Conversion from endoscopic endonasal trans-sphenoid surgery to microscopic or endoscopic assisted microsurgery
Although EETS provides superior visualization in most patients, conversion to a microscopic or endoscopic-assisted approach could be essential in selected patients for the safety of the patient. Reasons of conversion to microscopic technique in Zada et al. series were reoperations with scarring along with loss of anatomic landmarks especially in Cushing's disease and acromegaly. Atypical nasal and sphenoid anatomy, desire for binocular vision, difficulty visualizing sella/midline and bleeding were also reasons of conversion.[124] Significant invasion of cavernous sinus especially lateral to carotid artery could be indication for conversion.[125] Intraoperative bleeding can be controlled by clip or haemostatic agent.[46126]
Pituitary centre
Strategies to improve patient outcome and to reduce complications include establishing centers of excellence for pituitary tumor. More focused residency and fellowship training in EETS could also improve outcome.[96127]
Multi-modality treatment for giant and aggressive invasive tumors
Very aggressive surgical treatment in some giant and invasive tumor could increase complications. Multi-modality treatment could improve clinical outcome and reduce complications [Table 1]. Close collaboration of neurosurgeons with endocrinologists and radiation oncologists is essential for optimal treatment of patients with these challenging tumors.[128] Multimodality therapy such as Gamma knife, stereotactic radiotherapy, medical management, apart from endoscopic surgery, could be required for optimal tumor control.[32102129130] The octreotide long-acting release and lanreotide Autogel are used in acromegaly patients and were found to have similar efficacy for biochemical cure and tumor shrinkage as compared to surgery.[131]
Source of Support: Nil
Conflict of Interest: None declared
References
- Endoscopic treatment of the suprasellar arachnoid cyst. Neurol India. 2010;58:280-3.
- [Google Scholar]
- Combined endoscopic transsphenoidal-transventricular approach for resection of a giant pituitary macroadenoma. World Neurosurg. 2010;74:161-4.
- [Google Scholar]
- A new minimally invasive tubular brain retractor system for surgery of deep intracerebral hematoma. Neurol India. 2011;59:74-7.
- [Google Scholar]
- The neurosurgical anatomy of the sphenoid sinus and sellar floor in endoscopic transsphenoidal surgery. J Neurosurg. 2011;114:1319-30.
- [Google Scholar]
- Endoscopic anatomy of sphenoid sinus for pituitary surgery. Clin Anat. 2008;21:627-32.
- [Google Scholar]
- 3D modeling-based surgical planning in transsphenoidal pituitary surgery--preliminary results. Acta Otolaryngol. 2008;128:1011-8.
- [Google Scholar]
- Variations of endonasal anatomy: Relevance for the endoscopic endonasal transsphenoidal approach. Acta Neurochir (Wien). 2010;152:1015-20.
- [Google Scholar]
- Evaluation of early visual recovery in pituitary macroadenomas after endoscopic endonasal transphenoidal surgery: Quantitative assessment with diffusion tensor imaging (DTI) Acta Neurochir (Wien). 2011;153:831-42.
- [Google Scholar]
- Endoscopic sellar floor reconstruction with concha bullosa bone autograft and nasal septal flap: Technical case report. Minim Invasive Neurosurg. 2009;52:86-8.
- [Google Scholar]
- Transnasal trans-sphenoidal endoscopic repair of CSF leak secondary to invasive pituitary tumours using a nasoseptal flap. Pituitary. 2011;14:163-7.
- [Google Scholar]
- Endoscopic pedicled nasoseptal flap reconstruction for pediatric skull base defects. Laryngoscope. 2009;119:1067-75.
- [Google Scholar]
- Janus flap: Bilateral nasoseptal flaps for anterior skull base reconstruction. Otolaryngol Head Neck Surg. 2010;142:327-31.
- [Google Scholar]
- Nasoseptal “rescue” flap: A novel modification of the nasoseptal flap technique for pituitary surgery. Laryngoscope. 2011;121:990-3.
- [Google Scholar]
- Low-grade CSF leaks in endoscopic trans-sphenoidal pituitary surgery: Efficacy of a simple and fully synthetic repair with a hydrogel sealant. Acta Neurochir (Wien). 2011;153:815-22.
- [Google Scholar]
- Management of intra-operative cerebrospinal fluid leak following endoscopic trans-sphenoidal pituitary surgery. J Laryngol Otol. 2011;125:311-3.
- [Google Scholar]
- Endoscopic repair of high-flow cranial base defects using a bilayer button. Laryngoscope. 2010;120:876-80.
- [Google Scholar]
- Surgical repair of persisting CSF leaks following standard or extended endoscopic transsphenoidal surgery for pituitary tumor. Minim Invasive Neurosurg. 2010;53:55-9.
- [Google Scholar]
- Endoscopic, endonasal extended transsphenoidal, transplanum transtuberculum approach for resection of suprasellar lesions. J Neurosurg. 2007;106:400-6.
- [Google Scholar]
- [Endoscopic endonasal surgery for extrasellar tumors: Case presentation and its future perspective] No Shinkei Geka. 2009;37:229-46.
- [Google Scholar]
- Total septal preservation for sellar approach - paving the way for future flap reconstructions. Acta Otolaryngol. 2011;131:447-50.
- [Google Scholar]
- A novel approach allowing binostril work to the sphenoid sinus. Otolaryngol Head Neck Surg. 2008;138:531-2.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal approach through the bilateral nostrils for pituitary adenomas. Neurol Med Chir. 2009;49:1-7.
- [Google Scholar]
- A novel transnasal transsphenoidal speculum: A design for both microscopic and endoscopic transsphenoidal pituitary surgery. J Neurosurg. 2011;114:1380-5.
- [Google Scholar]
- [Minimally invasive neurosurgery for removal of pituitary adenomas by neuroendoscope aided with sellar floor reconstruction] Zhonghua Yi Xue Za Zhi. 2010;90:2342-4.
- [Google Scholar]
- Extended endoscopic endonasal approach to the skull base. Minim Invasive Neurosurg. 2009;52:114-8.
- [Google Scholar]
- Extended endoscopic approaches for midline skull-base lesions. Neurosurg Rev. 2009;32:309-19. discussion 318-9
- [Google Scholar]
- Endoscopic endonasal pituitary transposition for a transdorsum sellae approach to the interpeduncular cistern. Neurosurgery. 2008;62(3 Suppl 1):57-62. discussion 72-4
- [Google Scholar]
- Transsphenoidal pseudocapsule-based extracapsular resection for pituitary adenomas. Acta Neurochir (Wien). 2011;153:799-806.
- [Google Scholar]
- Surgical outcome of the endoscopic endonasal approach for non-functioning giant pituitary adenoma. J Clin Neurosci. 2011;18:71-5.
- [Google Scholar]
- Anatomical considerations for endoscopic endonasal skull base surgery in pediatric patients. Laryngoscope. 2010;120:1730-7.
- [Google Scholar]
- [Image-guided endoscopic transsphenoidal removal of pituitary adenoma] Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2005;40:41-4.
- [Google Scholar]
- Recent advances in pituitary tumor management. Curr Opin Endocrinol Diabetes Obes. 2011;18:278-88.
- [Google Scholar]
- Image-guided endoscopic transsphenoidal removal of pituitary tumours. J Otolaryngol Head Neck Surg. 2008;37:474-80.
- [Google Scholar]
- Endoscopic transnasal approach to the pituitary lesions using a navigation system (InstaTrak system): Technical note. Minim Invasive Neurosurg. 2002;45:120-3.
- [Google Scholar]
- A technical note on endonasal combined microscopic endoscopic with free head navigation technique of removal of pituitary adenomas. Neurosurg Rev. 2010;33:243-8. discussion 248-9
- [Google Scholar]
- Endoscopic endonasal transsphenoidal surgery using a skull reference array and laser surface scanning. Minim Invasive Neurosurg. 2008;51:244-6.
- [Google Scholar]
- Neuronavigation: Concept, techniques and applications. Neurol India. 2002;50:244-55.
- [Google Scholar]
- How to overcome the limitations to determine the resection margin of pituitary tumours with low-field intra-operative MRI during trans-sphenoidal surgery: Usefulness of Gadolinium-soaked cotton pledgets. Acta Neurochir. 2008;150:763-71. discussion 771
- [Google Scholar]
- Carotid artery visualization during anterior skull base surgery: A novel protocol for neuronavigation. Pituitary. 2010;13:215-22.
- [Google Scholar]
- Ultrasonic aspiration in neuroendoscopy: First results with a new tool. J Neurosurg. 2008;109:908-11.
- [Google Scholar]
- Emerging technology in intracranial neuroendoscopy: Application of the NICO Myriad. Neurosurg Focus. 2011;30:E6.
- [Google Scholar]
- Use of a side-cutting aspiration device for resection of tumors during endoscopic endonasal approaches. Neurosurg Focus. 2011;30:E13.
- [Google Scholar]
- Bone removal with a new ultrasonic bone curette during endoscopic endonasal approach to the sellar-suprasellar area: Technical note. Neurosurgery. 2010;66(3 Suppl Operative):E118.
- [Google Scholar]
- Pulsed laser-induced liquid jet for skull base tumor removal with vascular preservation through the transsphenoidal approach: A clinical investigation. Acta Neurochir (Wien). 2011;153:823-30.
- [Google Scholar]
- The use of the Olympus EndoArm for spinal and skull-based transsphenoidal neurosurgery. Minim Invasive Neurosurg. 2008;51:370-2.
- [Google Scholar]
- Use of a thrombin-gelatin haemostatic matrix in endoscopic endonasal extended approaches: Technical note. Acta Neurochir (Wien). 2009;151:69-77. discussion 77
- [Google Scholar]
- Value of high-definition imaging in neuroendoscopy. Neurosurg Rev. 2009;32:303-8. discussion 308
- [Google Scholar]
- Three-dimensional endoscopic pituitary surgery. Neurosurgery. 2009;64(5 Suppl 2):288-93. discussion 294-5
- [Google Scholar]
- [Videoendoscopic endonasal-transsphenoidal surgery of pituitary adenomas from a rhinological viewpoint] HNO. 2009;57:774-80.
- [Google Scholar]
- Perioperative cortisol can predict hypothalamus-pituitary-adrenal status in clinically non-functioning pituitary adenomas. J Endocrinol Invest. 2009;32:460-4.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal surgery for sellar tumors in children. Int J Pediatr Otorhinolaryngol. 2010;74:1298-302.
- [Google Scholar]
- Staged use of the transsphenoidal approach to resect superior third ventricular craniopharyngiomas. Minim Invasive Neurosurg. 2010;53:40-3.
- [Google Scholar]
- Combined simultaneous endoscopic transsphenoidal and endoscopic transventricular resection of a giant pituitary macroadenoma. Minim Invasive Neurosurg. 2008;51:306-9.
- [Google Scholar]
- Synchronous ventriculoscopic and microsurgical resection of complex craniopharyngiomas. Pediatr Neurosurg. 2009;45:434-6.
- [Google Scholar]
- Combined trans-sphenoidal and simultaneous trans-ventricular-endoscopic decompression of a giant pituitary adenoma: Case report. Acta Neurochir (Wien). 2009;151:843-7. discussion 847
- [Google Scholar]
- Endoscopic endonasal removal of pituitary adenomas with paraclival internal carotid artery invasion. ORL J Otorhinolaryngol Relat Spec. 2010;72:28-37.
- [Google Scholar]
- Extended transsphenoidal approach for surgical management of pituitary adenomas invading the cavernous sinus. J Neurosurg. 2008;108:26-36.
- [Google Scholar]
- Endoscopic transsphenoidal treatment in recurrent and residual pituitary adenomas--first experience. Minim Invasive Neurosurg. 2006;49:10-4.
- [Google Scholar]
- Hemorrhagic pituitary macroadenoma: Characteristics, endoscopic endonasal transsphenoidal surgery, and outcomes. Ann Surg Oncol. 2011;18:246-52.
- [Google Scholar]
- Delayed pituitary apoplexy in patient with advanced prostate cancer treated with gonadotrophin-releasing hormone agonists. J Clin Neurosci. 2010;17:1201-3.
- [Google Scholar]
- Endonasal endoscopic transsphenoidal chiasmapexy with silicone plates for empty sella syndrome: Technical note. Neurol Med Chir (Tokyo). 2005;45:428-32. discussion 432
- [Google Scholar]
- Expanded endoscopic endonasal approach for anterior cranial base and suprasellar lesions: Indications and limitations. Neurosurgery. 2009;64:677-87. discussion 687-9
- [Google Scholar]
- Endoscopic Vascular Decompression of the Trigeminal Nerve. Minim Invasive Neurosurg. 2011;54:110-4.
- [Google Scholar]
- Extended endoscopic endonasal approach for selected pituitary adenomas: Early experience. J Neurosurg. 2011;114:345-53.
- [Google Scholar]
- Extended endoscopic endonasal transsphenoidal approach for residual or recurrent craniopharyngiomas. J Neurosurg. 2009;111:578-89.
- [Google Scholar]
- Endoscopic pituitary surgery: A systematic review and meta-analysis. J Neurosurg. 2009;111:545-54.
- [Google Scholar]
- [Transphenoidal endoscopic approaches for pituitary adenomas: A critical review of our experience] Acta Otorrinolaringol Esp. 2011;62:25-30.
- [Google Scholar]
- [Pure endoscopic endonasal transsphenoidal approach for 375 pituitary adenomas] Zhonghua Wai Ke Za Zhi. 2010;48:1443-6.
- [Google Scholar]
- Outcomes and quality of life assessment in patients undergoing endoscopic surgery for pituitary adenomas. Br J Neurosurg. 2008;22:630-5.
- [Google Scholar]
- Microscopic versus endoscopic pituitary surgery: A systematic review. Laryngoscope. 2010;120:1292-7.
- [Google Scholar]
- Quality of postoperative course in children: Endoscopic endonasal surgery versus sublabial microsurgery. Acta Neurochir (Wien). 2011;153:843-9.
- [Google Scholar]
- [Transsphenoidal surgery for pituitary tumors from microsurgery to the endoscopic surgery: Single surgeon's experience] No Shinkei Geka. 2011;39:141-7.
- [Google Scholar]
- Analysis of transnasal endoscopic versus transseptal microscopic approach for excision of pituitary tumors. Am J Rhinol. 2008;22:649-52.
- [Google Scholar]
- Microscopic versus endoscopic transnasal pituitary surgery. Curr Opin Otolaryngol Head Neck Surg. 2010;18:8-14.
- [Google Scholar]
- Retrospective comparison of an endoscopic assisted versus a purely endoscopic approach to sellar tumour resection. J Otolaryngol Head Neck Surg. 2008;37:759-67.
- [Google Scholar]
- Purely endoscopic transsphenoidal surgery versus traditional microsurgery for resection of pituitary adenomas: Systematic review. J Otolaryngol Head Neck Surg. 2011;40:175-85.
- [Google Scholar]
- [Prospective comparative study on 50 patients between microsurgical sublabial transsphenoidal approach and endoscopic endonasal transsphenoidal approach] Neurocirugia (Astur). 2009;20:335-44. discussion 344-5
- [Google Scholar]
- Endoscopic approach for pituitary surgery improves rhinologic outcomes. Ann Otol Rhinol Laryngol. 2009;118:630-5.
- [Google Scholar]
- Nasal symptoms following endoscopic transsphenoidal pituitary surgery: Assessment using the General Nasal Patient Inventory. Neurosurg Focus. 2011;30:E12.
- [Google Scholar]
- Maximizing the extent of tumor resection during transsphenoidal surgery for pituitary macroadenomas: Can endoscopy replace intraoperative magnetic resonance imaging? J Neurosurg. 2010;112:736-43.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal surgery for growth hormone-secreting pituitary adenomas. Neurosurg Focus. 2010;29:E6.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal approach for growth hormone-producing pituitary adenomas. Preliminary results. Gac Med Mex. 2010;146:367-75.
- [Google Scholar]
- Endoscopy versus microsurgery: Results in a consecutive series of nonfunctioning pituitary adenomas. Neurochirurgie. 2009;55:607-15.
- [Google Scholar]
- Evidence of improved surgical outcome following endoscopy for nonfunctioning pituitary adenoma removal. Neurosurg Focus. 2011;30:E11.
- [Google Scholar]
- Changes in visual and oculomotor impairments after endoscopic endonasal transsphenoidal removal of pituitary adenomas. Vestn Oftalmol. 2009;125:23-7.
- [Google Scholar]
- Fully endoscopic transsphenoidal surgery for functioning pituitary adenomas: A retrospective comparison with traditional transsphenoidal microsurgery in the same institution. Surg Neurol. 2009;72:336-40.
- [Google Scholar]
- Microscopic endonasal transsphenoidal pituitary adenomectomy in the pediatric population. J Neurosurg Pediatr. 2011;7:501-9.
- [Google Scholar]
- Pure endoscopic transsphenoidal surgery for treatment of acromegaly: Results of 67 cases treated in a pituitary center. Neurosurg Focus. 2010;29:E7.
- [Google Scholar]
- Transsphenoidal surgery in patients with acromegaly: Operative strategies for overcoming technically challenging anatomical variations. Neurosurg Focus. 2010;29:E8.
- [Google Scholar]
- Outcomes after a purely endoscopic transsphenoidal resection of growth hormone-secreting pituitary adenomas. Neurosurg Focus. 2010;29:E5.
- [Google Scholar]
- Current state of the art in the diagnosis and surgical treatment of Cushing disease: Early experience with a purely endoscopic endonasal technique. Neurosurg Focus. 2007;23:E9.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal surgery: Surgical results of 228 pituitary adenomas treated in a pituitary center. Pituitary. 2010;13:68-77.
- [Google Scholar]
- Transsphenoidal pituitary surgery via the endoscopic technique: Results in 35 consecutive patients with Cushing's disease. Eur J Endocrinol. 2006;154:675-84.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal approach for pituitary adenomas: Technical aspects and report of casuistic. Arq Neuropsiquiatr. 2010;68:608-12.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal surgery for functional pituitary adenomas. Neurosurg Focus. 2011;30:E10.
- [Google Scholar]
- Sublabial transseptal vs transnasal combined endoscopic microsurgery in patients with Cushing disease and MRI-depicted microadenomas. Mayo Clin Proc. 2008;83:550-3.
- [Google Scholar]
- Endoscopic endonasal transsphenoidal approach for pituitary adenomas invading the cavernous sinus. J Neurosurg. 2010;112:99-107.
- [Google Scholar]
- Rhinologic outcomes of concurrent operation for pituitary adenoma and chronic rhinosinusitis: An early experience. Am J Rhinol. 2008;22:533-6.
- [Google Scholar]
- Defining the “edge of the envelope”: Patient selection in treating complex sellar-based neoplasms via transsphenoidal versus open craniotomy. J Neurosurg. 2011;114:286-300.
- [Google Scholar]
- Comparison of endoscopic and microscopic removal of pituitary adenomas: Single-surgeon experience and the learning curve. Neurosurg Focus. 2008;25:E10.
- [Google Scholar]
- Endoscopic transsphenoidal pituitary surgery: Evidence of an operative learning curve. Neurosurgery. 2010;67:1205-12.
- [Google Scholar]
- Training in endoscopic endonasal transsphenoidal surgery using a skull model and eggs. Acta Neurochir. 2010;152:1801-4.
- [Google Scholar]
- Making the transition from microsurgery to endoscopic trans-sphenoidal pituitary neurosurgery. Neurosurg Clin N Am. 2010;21:643-51. vi
- [Google Scholar]
- Endoscopic endonasal approach for pituitary adenoma: Surgical complications in 301 patients. Pituitary. 2011;14:174-83.
- [Google Scholar]
- Postoperative diabetes insipidus after transsphenoidal resection of pituitary tumor. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2007;42:199-201.
- [Google Scholar]
- Predictors and incidence of central diabetes insipidus after endoscopic pituitary surgery. Neurosurgery. 2008;62:71-8. discussion 78-9
- [Google Scholar]
- Diabetes insipidus after pituitary surgery: Incidence after traditional versus endoscopic transsphenoidal approaches. Am J Rhinol. 2001;15:377-9.
- [Google Scholar]
- Cerebrospinal fluid rhinorrhea following trans-sphenoidal pituitary macroadenoma surgery: Experience from 592 patients. Clin Neurol Neurosurg. 2008;110:570-9.
- [Google Scholar]
- Cerebrospinal fluid fistula after endoscopic transsphenoidal surgery: Experience in a spanish center. Arq Neuropsiquiatr. 2010;68:414-7.
- [Google Scholar]
- Capsule plication as a protective measure against post-operative intracapsular haematoma formation following trans-sphenoidal removal of pituitary macroadenoma. Acta Neurochir (Wien). 2008;150:797-802. discussion 802
- [Google Scholar]
- Challenging reconstructive techniques for skull base defect following endoscopic endonasal approaches. Acta Neurochir (Wien). 2011;153:807-13.
- [Google Scholar]
- Endoscopic, endonasal resection of craniopharyngiomas: Analysis of outcome including extent of resection, cerebrospinal fluid leak, return to preoperative productivity, and body mass index. Neurosurgery. 2012;70:110-23. discussion 123-4
- [Google Scholar]
- Technique and outcome of endoscopy-assisted microscopic extended transsphenoidal surgery for suprasellar craniopharyngiomas. J Neurosurg. 2011;114:1338-49.
- [Google Scholar]
- Extracranial complications of endoscopic transsphenoidal sellar surgery. J Otolaryngol Head Neck Surg. 2010;39:309-14.
- [Google Scholar]
- Isolated sphenoid sinusitis or mucocele: A potential complication of endonasal transsphenoidal surgery. J Neurooncol. 2009;91:63-7.
- [Google Scholar]
- Prevention and cure sinusitis complicated by endoscopic transnasal approach in surgical treatment of pituitary adenoma. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2010;24:353-5.
- [Google Scholar]
- Endonasal versus supraorbital keyhole removal of craniopharyngiomas and tuberculum sellae meningiomas. Neurosurgery. 2009;64()(5 Suppl 2):269-84. discussion 284-6
- [Google Scholar]
- Olfactory changes after endoscopic pituitary tumor resection. Otolaryngol Head Neck Surg. 2010;142:95-7.
- [Google Scholar]
- Intraoperative conversion from endoscopic to microscopic approach for the management of sellar pathology: Incidence and rationale in a contemporary series. World Neurosurg. 2010;73:334-7.
- [Google Scholar]
- Transcranial approach to pituitary adenomas invading the cavernous sinus: A modification of the classical technique to be used in a low-technology environment. Surg Neurol Int. 2010;1:ii:25.
- [Google Scholar]
- A new technique for management of intercavernous sinus bleeding with titanium clips in transsphenoidal surgery. Neurol India. 2010;58:847-51.
- [Google Scholar]
- The role of outcomes data for assessing the expertise of a pituitary surgeon. Curr Opin Endocrinol Diabetes Obes. 2010;17:369-76.
- [Google Scholar]
- Endonasal transsphenoidal surgery and multimodality treatment for giant pituitary adenomas. Clin Endocrinol (Oxf). 2010;72:512-9. Epub 2009 Jun 25
- [Google Scholar]
- Comparison of octreotide LAR and lanreotide autogel as post-operative medical treatment in acromegaly. 2011. Pituitary. Available from: http://www.springerlink.com/content/d41g5j444u711301/fulltext.pdf
- [Google Scholar]






