Translate this page into:
Solitary cerebellous metastasis after prolonged remission in a case of uterine cervical adenocarcinoma
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intracranial metastasis of a uterine cervical carcinoma is a very rare occurrence. These metastases are characteristically multiple, supra-tentorial, associated with multiple systemic dissemination, usually occur relatively late in the course of the disease, and are most often seen in squamous carcinomas. We present an unusual case which defied these characteristics. This patient was in long-term remission (11 years), presented with a solitary cerebellous metastases, had no evidence of other systemic spread, and the pathology was an adenocarcinoma. We present this rare case with interesting clinical ramifications. This is probably the longest duration of remission prior to the metastasis in the published literature.
Keywords
Adenocarcinoma
cerebellous metastasis
uterine cervical squamous cell carcinoma
Introduction
Cancer of the uterine cervix (CUC) is one of the leading cancer in women and the most common cancer among all sites in both sexes in India.[1] It has been estimated that 100,000 new cases of CUC occur in India every year.[1] CUC has a very low potential for metastases (<10%).[2] Metastases have a proclivity for certain sites, namely retroperitoneal lymph nodes, lung, and bone.[3] Cerebral metastases, rarely reported, have a low incidence (0.5% to 1%) and usually occur late as a component of disseminated disease with systemic involvement.[2] Most (two-third) are multiple and supra-tentorial.[2] Cerebellum is a very unusual site for metastasis.[2–4] The median interval from primary diagnosis to metastases has been described at 18 months.[3] These tumors are usually poorly differentiated[23] and the most common histopathology is proven to be the squamous tumors with very few reported cases of adenocarcinomas.[3]
We report an unusual presentation of a solitary cerebellar metastasis after 11 years remission. The lesion was an adenocarcinoma with extensive mucoid differentiation with no recurrence at long-term follow up.
Case Report
A 51-year-old lady presented with raised intracranial pressure since 3 weeks. She had no neurological signs on examination. Prior history of the uterine cervical adenocarcinoma FIGO stage IB1 was present, 11 years ago for which she had undergone a radical hysterectomy with bilateral salpingo-oophorectomy and pelvic lymph node clearance. Lymph nodes taken from both common, external and internal iliac groups and the obturator nodes revealed no metastases. She underwent adjuvant radiotherapy-30 fractions of 200 cGy each adding to a total of 60 Gray.
Brain MRI done at presentation revealed [Figures 1a–c] a well-defined, solitary lesion of the left cerebellar hemisphere. A systemic MRI survey did not reveal any other metastases. She underwent a lateral suboccipital craniectomy and complete excision of the lesion. Intraoperatively the lesion was encapsulated, with well-defined planes and contained a whitish yellow mucoid material. Post-operative MRI revealed complete excision of the lesion. The histopathology [Figures 2a–c] revealed features of a mucinous papillary adenocarcinoma with abundant mucin secretion. The patient underwent adjuvant whole brain radiotherapy [WBRT] and has been on follow up for 3 years with no recurrence of the lesion.
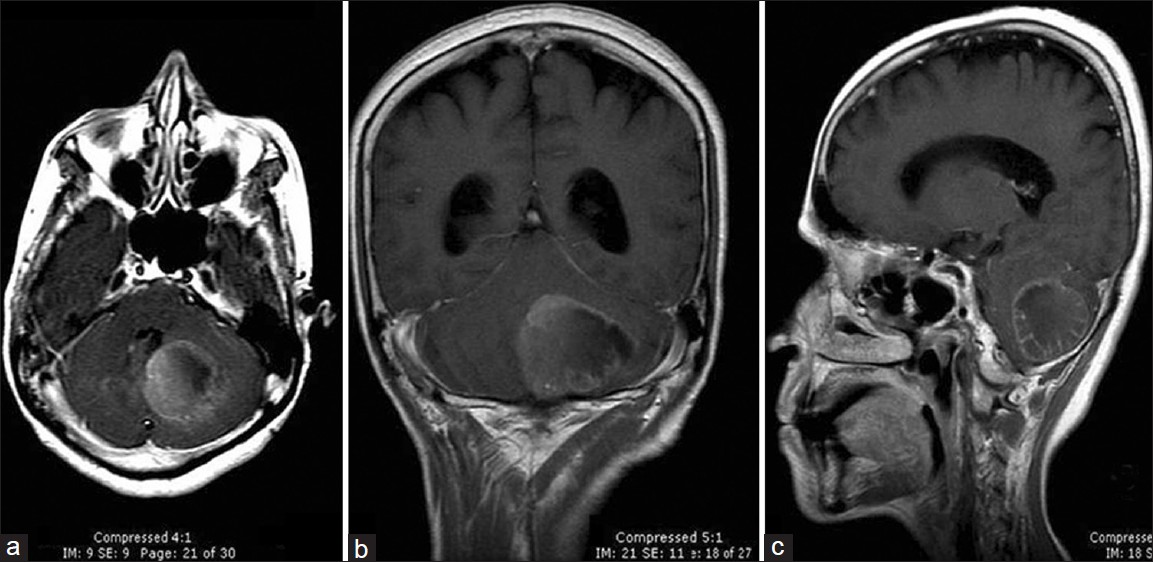
- (a-c) Pre-operative MRI of the brain demonstrating the lesion. Axial (a), coronal (b) and sagittal (c) images of T1W post-contrast images revealed a heterogeneous enhancement in a well-circumscribed intra-axial lesion in the left cerebellar hemisphere measuring 3.2 × 3.8 × 4.3 cm. The lesion is seen abutting the left lateral recess of the fourth ventricle with mass effect
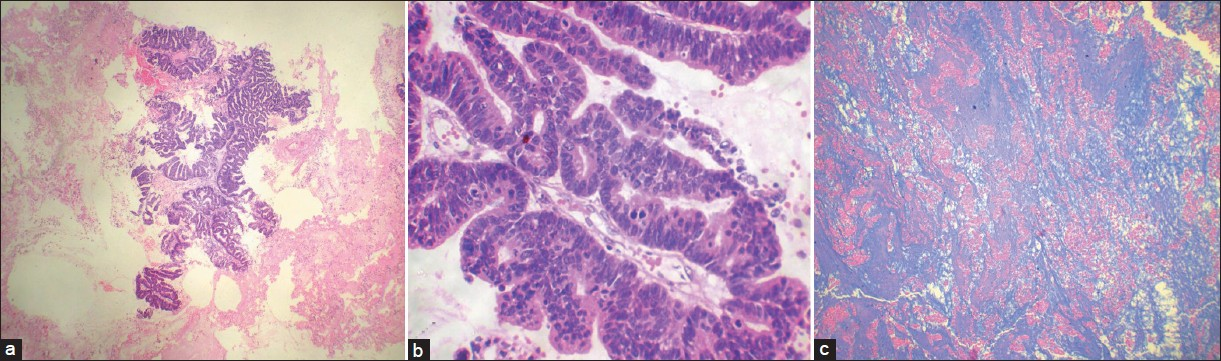
- (a-c) Paraffin section showing a metastatic adenocarcinoma [hematoxylin and eosin (a) ×40; (b) ×100]. Abundant mucin secretion visualized [Alcian Blue stain ×100]
Discussion
The incidence of metastasis in CUC in reviews published has ranged from 0.416% to 0.76%.[5–7] The time interval of metastases after diagnosis of CUC is reported from 8 weeks to 8 years (longest),[5] with the median time for manifestation being 18 months.[4] Unusual shorter latent periods of 1-5 weeks have been reported.[4] An unusually long remission of 11 years as in this patient has not been reported earlier in the literature. No association between the histology and time interval has ever been ascertained.[2–10]
Hematogenous and vertebral venous system as routes of dissemination have been implicated.[27] Possible association between the size of the primary and the propensity to metastasize has been reported.[7]
The more frequent supra-tentorial occurrence of the metastases is probably related to the spatial characteristics of the lesion and vascularity.[8] There are very few clinical reports of brain involvement without detectable systemic involvement.[8] Only about one third of all reported cases have had lesions in the posterior fossa and solitary lesions there are even rarer.[2] The presence of tumor cells in cerebral vasculature has been found in patients without obvious metastases leading to implicate other factors in the pathogenesis such as host immune response, neo-vascularization, and tumor cell properties.[3]
The most common histopathology of the metastatic lesion has been reported as the squamous cell carcinoma with rare incidence of adenocarcinomas.[2–6] The relative occurrence of the different cellular histology would explain the corresponding incidence of metastases in the adenocarcinoma group.[9]
The primary histology does not have prognostic significance to predict metastases.[8] The current recommended treatment modalities for cerebral metastases are surgery followed by adjuvant radio [WBRT or stereotactic radiosurgery (SRS)] or chemoradiotherapy.[2–10] Management depends on the systemic disease, number metastases, and the clinical condition of the patient. A single lesions surgery followed by radiotherapy is reported to result in a long recurrence free survival of 6 years[10] and in another patient who survived 10 years following surgery for a solitary metastasis.[7] The median survival with surgery followed by radiotherapy has been found to be more effective than direct radiotherapy alone.[8] Palliative therapy – steroids and WBRT – is recommended in multiple intracranial lesions with multi-organ involvement.[8] SRS has been used as a treatment modality and may be as effective for small and inaccessible lesions.[8]
The overall survival in patients with CUC has been dismal, around 34% (irrespective of the stage) in one large series.[1] Long-term survival rates in metastases are typically very rare[2–9] but have been reported (6 years and 10 years).[710] Prognosis in a solitary cerebral metastasis is usually poor in view of the systemic involvement of the tumor[2] without which the outcome is considered favorable.[3] This patient has been on follow up for over 40 months with no evidence of any further metastases. A good post-operative survival in this case is attributed to a single metastasis, no systemic involvement, and complete surgical excision with adjuvant post-operative radiotherapy.
Conclusions
The diagnosis of a solitary, cerebellous metastasis from a primary CUC adenocarcinoma preceded by a very long remission is noteworthy. This case disproves several standard beliefs, namely the histology, single metastasis to the posterior fossa in the absence of other systemic metastases, protracted period of remission prior to metastasis, and prolonged survival after definitive surgery. Surgical excision especially for solitary lesions without systemic involvement results in favorable outcome. A very high degree of suspicion is warranted in patients with prior diagnosis of CUC and also caution is to be rendered in prognosticating since prolonged remission both prior to and after metastasis does occur.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Incidence, mortality and survival in cancer of the cervix in Bangalore, India. Br J Cancer. 1995;71:1348-52.
- [Google Scholar]
- Cerebellous metastases in patients with uterine cervical cancer.Two cases reports and review of the literature. Cancer Radiother. 2003;7:317-20.
- [Google Scholar]
- Surgical resection of solitary brain metastasis from cervical cancer. Int J Gynecol Cancer. 2003;13:368-70.
- [Google Scholar]
- Rapid manifestation of CNS metastatic disease in a cervical carcinoma patient: A case report. Oncology. 2007;73:273-6.
- [Google Scholar]
- Rapid growth of cervical cancer metastasis in the brain. J Clin Neurosci. 2010;17:1211-2.
- [Google Scholar]
- Cerebral metastasis in patients with uterine cervical cancer. Jpn J Clin Oncol. 1998;28:27-9.
- [Google Scholar]
- Intracranial metastases from carcinoma of the cervix: Report of 4 cases and review of the literature. J HK Coll Radiol. 2005;8:112-6.
- [Google Scholar]
- Brain metastasis from uterine cervical cancer. J Obstet Gynaecol Res. 2010;36:701-4.
- [Google Scholar]
- Carcinoma of the uterine cervix: A review of its pathology and commentary on the problem in Malaysians. Malays J Pathol. 1999;21:1-15.
- [Google Scholar]






