Translate this page into:
Midbrain cysticercal cyst
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 26-years-old gentleman presented with history of fever, headache, double vision and drooping of both eyelids of three days duration. Examination revealed bilateral ptosis and restriction of upward gaze. The pupils were 4 mm in diameter, and sluggishly reacting to light. Visual acuity was 6/18 in both eyes. Both optic discs were hyperemic. Rest of the neurological examination was normal. An MRI of brain showed a single ring shaped lesion in midbrain. The lesion was cystic with a small solid nodule and perilesional edema. The wall of the cyst was isointense on T1 and T2. Post contrast MRI showed enhancement of cyst and small nodule [Figure 1]. The imaging findings were characteristic of a cysticercal cyst with a scolex. The patient was treated conservatively and no specific medication was given. He improved spontaneously, and at follow up, three months after onset of symptoms he had diplopia on looking toward right, though no extraocular muscle palsy was evident on examination.
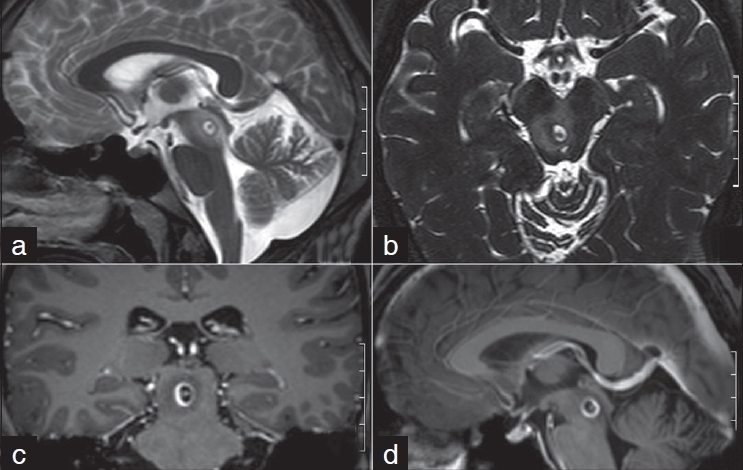
- MRI brain: T2 sagittal (a), CISS 3D (b), postcontrast coronal (c) and sagittal (d) showing a single ring lesion with an enhancing scolex in midbrain with perilesional edema.
Neurocysticercosis (NCC) is the most common parasitic disease of the nervous system in humans.[1] Symptomatic NCC results from a combination of factors, including the number, stage, and location of the parasites within the nervous system, as well as the severity of the host's immune response against the parasites.[2] NCC commonly presents with seizures, raised intracranial tension, and dementia. The unusual location of the cysts may result in uncommon neurological manifestations.[3]
The causes of third nerve palsies in NCC are hydrocephalus, arachnoiditis in the interpeduncular cisterns, ischemia of midbrain, and intraparenchymal cyst within midbrain.[3] There are few reports of NCC within the midbrain. The following midbrain syndromes are described due to NCC: Isolated third cranial nerve palsy, recurrent third cranial nerve palsy, isolated bilateral ptosis, dorsal midbrain syndrome, and Claude's syndrome.[34] Our case presented with dorsal midbrain syndrome.
Diagnosis of NCC is typically made on the basis of characteristic neuroimaging findings. Cystic lesions showing the scolex on CT or MRI are diagnostic of NCC.[2] The imaging findings were characteristic of NCC and no further diagnostic modality was used in our case. There is evidence that single enhancing lesion represents degenerating cysts and does not require antiparasitic treatment. These patients are likely to do well independently of whether antiparasitic therapy is given.[1] Our patient also did not receive any treatment and improved spontaneously.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Current consensus guidelines for treatment of neurocysticercosis. Clin Microbiol Rev. 2002;15:747-56.
- [Google Scholar]
- Neurocysticercosis: Updated concepts about an old disease. Lancet Neurol. 2005;4:653-61.
- [Google Scholar]





