Translate this page into:
Unusual features in chronic inflammatory demyelinating polyneuropathy: Good outcome after prolonged ventilatory support
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Severe respiratory muscle paralysis and ventilatory failure is rare in chronic inflammatory demyelinating polyneuropathy (CIDP). We report a 14 year child who presented with respiratory failure, bulbar and multiple cranial nerves involvement along with bilateral phrenic nerve paralysis. He was diagnosed with CIDP after electrophysiological evaluation. He required AMBU ventilation for about 4 months (including domiciliary use), after which he recovered significantly. Along with several unusual features of CIDP, this report highlights good example of steady basic intensive care to save lives and rewarding outcome of prolonged respiratory support, provided by AMBU ventilation which is a rather primitive, but inexpensive device.
Keywords
AMBU ventilation
bulbar palsy
chronic inflammatory demyelinating polyneuropathy
phrenic nerve palsy
Introduction
Chronic inflammatory demyelinating polyneuropathy (CIDP) is immune-mediated, sensory-motor, peripheral neuropathy causing significant disability. Severe respiratory muscle paralysis and ventilatory failure is rare, but has recently been described in patients of CIDP.[12] We report a patient of CIDP presenting with several unusual features including phrenic nerve involvement and respiratory failure. He required AMBU ventilation for 4 months and recovered significantly. Through this report we wish to highlight an impressive example of steady basic intensive care and rewarding outcome of prolonged respiratory support provided by AMBU ventilation which is a rather primitive but an inexpensive device.
Case Report
A 14-year-old boy presented in neurology emergency, with history of progressive quadriparesis since 1 year. Weakness was initially confined only to upper limbs and in another 2 weeks involved the lower limbs. Over next 3 months, he lost the ability to walk, became bed bound and required assistance for all his activities of daily living. During this period, there was severe, diffuse loss of muscle mass in whole body. About 3 weeks prior to reporting, he developed severe breathlessness and nasal twang in voice along with nasal regurgitation of food and fluids .
On examination he was restless. There was fever with tachycardia and tachypnea. Accessory muscles of respiration were active and paradoxical respiratory movements were present. The single breath count was between seven and ten. Cognition was intact. There was paralysis of 9th, 10th, 11th, and 12th cranial nerves. Gross wasting of limb and trunk muscles was present. There was grade 3/5 power at both hip and knee joints with bilateral foot drop, grade 2/5 power at both shoulder and elbow joints with bilateral wrist drop. Severe weakness of trunk and neck muscles along with generalized hypotonia and areflexia was present. Sensory examination revealed impairment of posterior column sensations. Systemic examination was unremarkable.
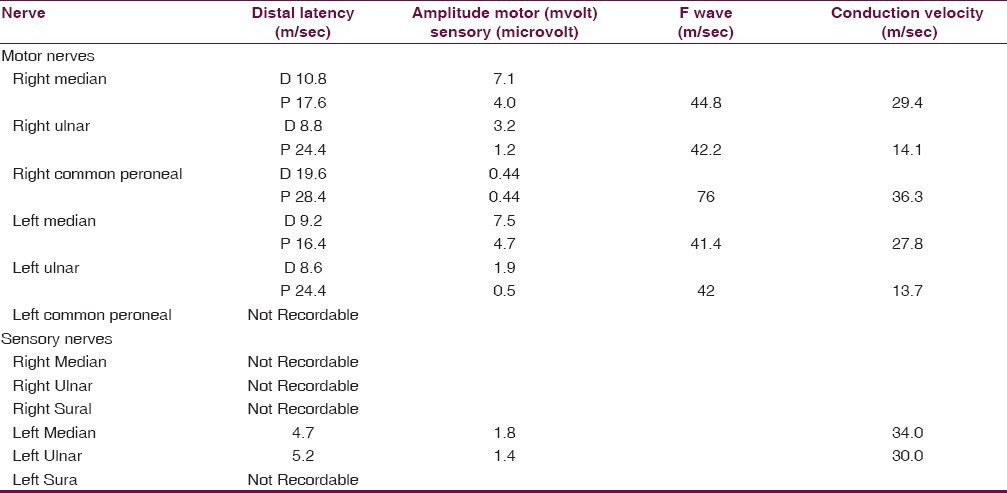
Hematology and serum biochemistry were normal. The serum creatine phosphokinase was normal (110 U/L) and needle EMG did not show any myogenic potentials. Nerve conduction studies [Table 1] showed prolonged distal latencies, conduction block, decreased conduction velocities, prolonged F-wave, and decreased motor action potentials of the median, ulnar and common peroneal nerves, suggesting demyelinating type of neuropathy. Electrophysiologically definite and clinically typical CIDP was considered as per the revised criterias published by the Peripheral Nerve Society and by the European Federation of Neurology.[3]
The chest X-ray revealed elevated domes of diaphragm suggesting bilateral phrenic nerve palsy which was later confirmed by fluoroscopy. Cerebrospinal fluid examination showed elevated proteins (120 mg/dL) and five lymphocytes. The vasculitis and hepatorenal profile, Venereal Disease Research Laboratory test, and Human Immunodeficiency Virus serology were negative. Serum electrophoresis was negative for M band and there was normoblastic erythropoiesis in bone marrow aspiration smear.
He was immediately intubated and ventilated by manual AMBU ventilation. A course of intravenous immunoglobulin was given, along with antibiotics. After ensuring adequate control of infections he was started on oral corticosteroids (1 mg/kg body weight). Due to financial constraints he remained on continuous AMBU ventilation for 6 weeks, after which he required it only intermittently (4-5 hrs/day) to maintain adequate oxygen saturation. Relatives of the patient were trained to provide accessory care like nutrition, physiotherapy of chest and limbs, throat suction, and care of tracheostomy tube under supervision of respective experts. Later they were also trained to use an ambubag device and ventilate the lungs at rate of 15- 16 /min. After 2 months of hospital stay there was a significant improvement in respiratory effort and motor power, he could stand and walk with minimal assistance. He remained on tracheostomy care and required domiciliary, intermittent AMBU ventilation. Over another 2 months patient was completely weaned from the AMBU ventilation and his tracheostomy tube was removed. Oral corticosteroids were tapered and withdrawn. Presently, the patient can breathe normally and perform all activities of daily living independently.
Discussion
The present case report had several interesting and unusual aspects. The most important being the remarkable recovery with prolonged AMBU ventilation in spite of delayed presentation. The age of onset of disease in our patient was 13 years, which is rare as CIDP has higher prevalence in adults as compared to those with age less than 19 years.[4] The current case had onset of weakness from upper limbs, which underscores the fact that neuropathy in case of CIDP may not always be the length-dependent process. Probably due to severe muscle wasting, which is not common in patients with CIDP, except with concomitant myopathy, the referral diagnosis of spinal muscular atrophy was earlier entertained.[5]
Our patient had clinical involvement of lower cranial nerves. Cranial neuropathy is uncommon (5%) in CIDP.[6] Thickening and enhancement of multiple cranial nerves on cranial magnetic resonance imaging in diagnosed cases of CIDP is reported, which may be silent clinically.[7] This patient demonstrated clinical and radiological evidence of the rare association of CIDP with phrenic nerve palsy, resulting in diaphragmatic paralysis and respiratory failure.[2] It is important to observe this condition, because phrenic nerve palsy is critical when bilateral or when it develops in patients with preceding respiratory diseases. Immunoadsorption plasmapheresis is the most effective treatment for CIDP, especially in patients with serious complications like phrenic nerve palsy, but it is not widely accessible, it is invasive and requires considerable expertise. However, as evident from the present case, CIDP may also be responsive to treatment with intravenous immunoglobulins or steroids, which is easily available.[3]
Respiratory failure in CIDP is exceptional and its early recognition may prevent significant morbidity and mortality. Successful use of AMBU ventilation for such a long period has never been reported before. However, manual AMBU ventilation has been reported in a case of Guillain-Barre syndrome for 18 days prior to availability of mechanical ventilator.[8] The current report does not intend to endorse the concept of AMBU ventilation at home as an alternative to in-hospital ventilator support. However, in developing countries advanced medical facilities like mechanical ventilatory and critical care support are not easily available or affordable. Under these circumstances the utility of AMBU ventilation cannot be underestimated. This is cheap, effective, and dependable after a proper training, and can be safely used as a domiciliary device in desperate situations.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Chronic inflammatory demyelinating polyneuropathy and respiratory failure. J Neurol. 2005;252:1235-7.
- [Google Scholar]
- Chronic inflammatory demyelinating polyradiculopathy: An atypical pediatric case complicated with phrenic nerve palsy. Turk J Pediatr. 2007;49:210-4.
- [Google Scholar]
- European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society - First Revision. Eur J Neurol. 2010;17:356-63.
- [Google Scholar]
- Prevalence and incidence rates of chronic inflammatory demyelinating polyneuropathy in the Japanese population. J Neurol Neurosurg Psychiatry. 2008;79:1040-3.
- [Google Scholar]
- Progressive chronic inflammatory demyelinating polyneuropathy in a child with central nervous system involvement and myopathy. Coll Antropol. 2006;30:945-9.
- [Google Scholar]
- Neurophysiological evaluation of trigeminal and facial nerves in patients with chronic inflammatory demyelinating polyneuropathy. Muscle Nerve. 2007;35:203-7.
- [Google Scholar]
- Magnetic resonance imaging findings in chronic inflammatory demyelinating polyneuropathy with intracranial findings and enhancing, thickened cranial and spinal nerves. Australas Radiol. 2007;51:21-4.
- [Google Scholar]
- Manual AMBU ventilation is still relevant in developing countries. QJM. 2008;101:990-1.
- [Google Scholar]






