Translate this page into:
Tuberculous brain abscesses: Case series and review of literature
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
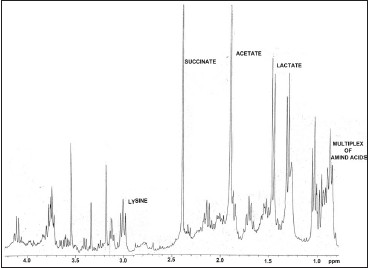
Tuberculous brain abscess (TBA) is a rare but serious condition. It resembles a pyogenic brain abscess clinically and radiologically and poses a problem in diagnosis and treatment. A final diagnosis is established by smear or culture demonstration of acid fast bacilli (AFB) within the abscess. Here, we report four such cases in our five-year study on brain abscesses, along with the different diagnostic modalities used.
Materials and Methods:
A total of 75 brain abscess pus specimens were collected during neurosurgery, either by burr hole or by craniotomy. These specimens were further subjected to Gram stain, Ziehl-Neelsen (ZN) stain, and conventional microbiological culture. Only those cases which showed presence of AFB on ZN stain along with the growth of Mycobacterium tuberculosis were considered as TBAs. Such TBA cases were further presented along with their In vitro Proton Magnetic Resonance (MR) Spectroscopic findings.
Results:
Of these four patients, three were males. Though this condition is more commonly seen in immunocompromised patients, three of the patients in this study were immunocompetent. All the four pus specimens showed presence of AFB in the ZN stain. Three of them grew M. tuberculosis as sole isolate. The fourth case was of concomitant tuberculous and pyogenic brain abscess. In vitro Proton MR spectroscopy of the pus specimens showed absence of multiple amino acids at 0.9 ppm, which was found to be hallmark of TBA. One patient died of four.
Conclusions:
TBA always poses a diagnostic dilemma. ZN stain and conventional microbiological culture for Mycobacteria always help to solve this dilemma. In vitro Proton MR Spectroscopy also seems to have the diagnostic utility.
Keywords
Brain abscess
pyogenic
tuberculous MR Spectra
Introduction
Tuberculous brain abscess (TBA) is a rarely reported form of central nervous system (CNS) tuberculosis.[1] TBA is a focal collection of pus containing abundant acid fast bacilli (AFB) surrounded by a dense capsule consisting of vascular granulation tissue.[2] TBA always poses a diagnostic dilemma as they are difficult to differentiate from pyogenic brain abscesses, tuberculous meningitis, and tuberculoma on the basis of clinical, laboratory, and roentgenographic information.[1] Whitener,[1] in his excellent review, had laid down the diagnostic criteria for TBA. The present study reports four cases of TBA along with comparative analysis of other TBA cases from the available literature.
Materials and Methods
During the 5-year study on brain abscesses, pus specimen was collected during neurosurgery either by burr hole or by craniotomy. This was then sent to Department of Microbiology for the subsequent workup after obtaining proper consent. This study was performed after obtaining necessary ethical clearance from the institutional ethical committee.
Gram and Ziehl-Neelsen (ZN) stains were performed immediately. Aerobic, anaerobic, and fungal cultures were put up using conventional methods.[3] Pus specimens were also inoculated on Lowenstein Jensen's medium and incubated at 37°C for 6 to 8 weeks. Colonies obtained were confirmed to be acid fast by ZN and then were identified by conventional methods such as rate of growth, pigment production, niacin accumulation, nitrate reduction test, and sensitivity to paranitrobenzoic acid (500μg/ml).[3]
In three TBA cases, 100 μl of pus sample was loaded in 5 mm NMR tube and deuterium oxide (D2O) (Armar Chemicals, Switzerland) was added to make approximate volume of 0.6 ml, and then subjected to In vitro Proton MR Spectroscopy (1H MRS) using Mercury plus Varian 300 MHz (7.05 T) nuclear MR spectrometer. After the NMR analysis (256 scans), the different peaks obtained were noted. Referencing was done with the water peak at 4.8 ppm. The interpretation of peaks was done according to the available literature.[45] The spectra of pus which yielded Mycobacterium tuberculosis were further compared with spectra of pus that yielded pyogenic organisms.
Results
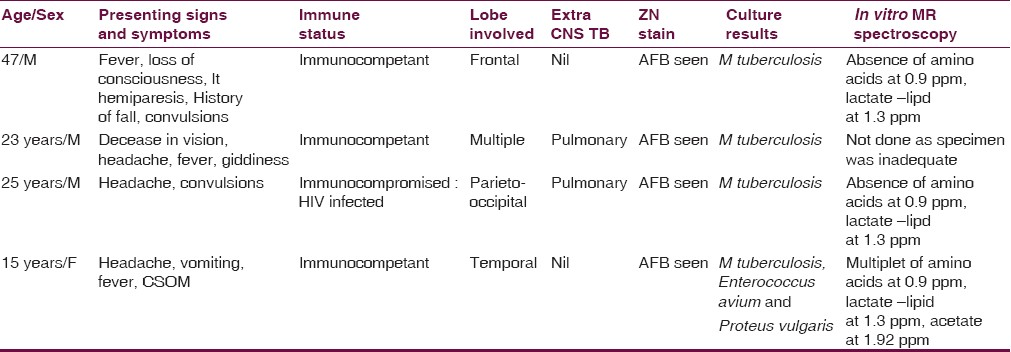
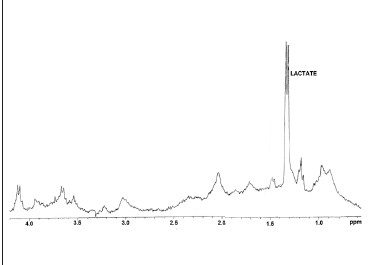
Of 75 pus specimens, ZN stain revealed presence of AFB in four (5.3%). Three pus specimens grew M. tuberculosis as the sole pathogen causing the brain abscess. In one case, along with M. tuberculosis, pus specimen showed growth of Enterococcus avium and Proteus vulgaris. Table 1 shows all the details of the patients encountered in the present study. Of these four cases, three were immunocompetent, while one patient was infected with Human Immunodeficiency Virus(HIV). Two of the pus specimens which yielded pure growth of M. tuberculosis subjected to in vitro 1H MRS showed complete absence of multiplet of amino acids-lipids at 0.9 ppm and lactate + lipid at 1.3 ppm [Figure 1a]. Pus from pyogenic brain abscesses (anaerobic) showed presence of multiplet of amino acids-lipids at 0.9 ppm along with presence of lactate + lipid at 1.3 ppm, acetate at 1.92 ppm, and succinate at 2.4 ppm [Figure 1b]. However, the pus specimen which yielded M. tuberculosis along with E. avium + P. vulgaris showed spectra similar to pyogenic brain abscess.
-
In vitro 1H MRS of the pus specimen which grew Mycobacterium tuberculosis on culture
-
In vitro 1H MRS of the pus specimen which grew anaerobe on culture
Discussion
M. tuberculosis is a rare cause of brain abscess; however, this organism should be considered in patients with disseminated tuberculosis or in individuals from areas where tuberculosis is endemic.[2] The present study noticed four (5.4%) TBA cases in five-year study on brain abscesses. In all these four cases, there was an evidence of pus within the brain and bacteriological proof of AFB in the pus by microscopy as well as by culture. In 1978, Whitner[1] reported a case of TBA and reviewed 57 similar cases in the world literature. He found that only 16 of the 57 cases could be considered as verified TBAs in terms of the following three criteria: 1. Macroscopic evidence from surgical or autopsy material of true abscess formation within the brain substance, characterized by cavity formation with central pus; 2. Sufficient histological description to assure that the inflammatory reaction in the abscess wall was composed predominantly of vascular granulation tissue containing acute and chronic inflammatory cells particularly polymorphonuclear leukocytes; and 3. Proof of tuberculosis origin by either a positive culture of the pus for M. tuberculosis or demonstration of acid-fast organisms in the pus or abscess wall. After Whitner[1] reviewed the world literature, isolated cases of TBAs have been reported.[6–17] In most of these cases, proof of tuberculosis origin was by either a positive culture of the pus for M. tuberculosis or demonstration of acid-fast organisms in the pus, except in the study by Kaushik et al.,[15] the diagnosis was confirmed by Polymerase chain reaction (PCR) for M. tuberculosis MPB64. Thus, newer techniques like PCR may provide useful tool for diagnosis of tuberculosis from paucibacillary specimens like pus in which conventional methods may show low sensitivity. Even in the present study, a new technique, In vitro 1HMRS, was evaluated for the diagnosis of TBA. Absence of multiplet of amino acids-lipids at 0.9 ppm seems to be a hallmark of TBAs. Similar findings have been reported in the literature.[1819] An attempt was made to compare these spectra with the pus specimen, which showed pure growth of anaerobe (pyogenic brain abscess). Pus specimens which showed the presence of anaerobes on culture revealed the presence of multiplet at 0.9 ppm, along with lactate-lipid at 1.3 ppm, acetate at 1.92 ppm, and succinate at 2.4 ppm [Figure 1a and b]. The case of concomitant tuberculous and pyogenic brain abscess showed spectra similar to pyogenic brain abscess. However, succinate (marker for anaerobes) peak was absent suggesting that the pus specimen may have facultative anaerobes. As there are no major peaks in TBA except that of lactate-lipid, the total spectra were masked by the pyogenic abscess spectra. However, the Gram stain, ZN stain, and gold standard conventional culture gave the complete etiological diagnosis.
Whitener's[1] review of 16 cases also revealed the following common features in TBA: 1. Frequent occurrence of TBA in the third and fourth decade of life; 2. A 35% incidence of multiple brain abscesses; 3. Predominant supratentorial location of the abscess in the frontal lobe; 4. Evidence of extra CNS tuberculosis in 85% cases; and 5. Occurrence of TBA despite antituberculous treatment and presentation with rapidly progressive neurological deficit.
Contrary to Whitener's[1] observations, one of our patients was a 15-year-old girl. Table 2 clearly shows that TBA can occur at any age. Of four cases in the present study, one (25%) of the patients presented with multiple brain abscesses involving temporal, parietal, and occipital lobe. Remaining three cases had a solitary abscess involving frontal, temporal, and parietal lobe. Multiple TBA is rare, with only a few reports appearing in the literature.[1720] Table 2 also shows that TBA can occur in any part of brain involving the ventricles.[10]
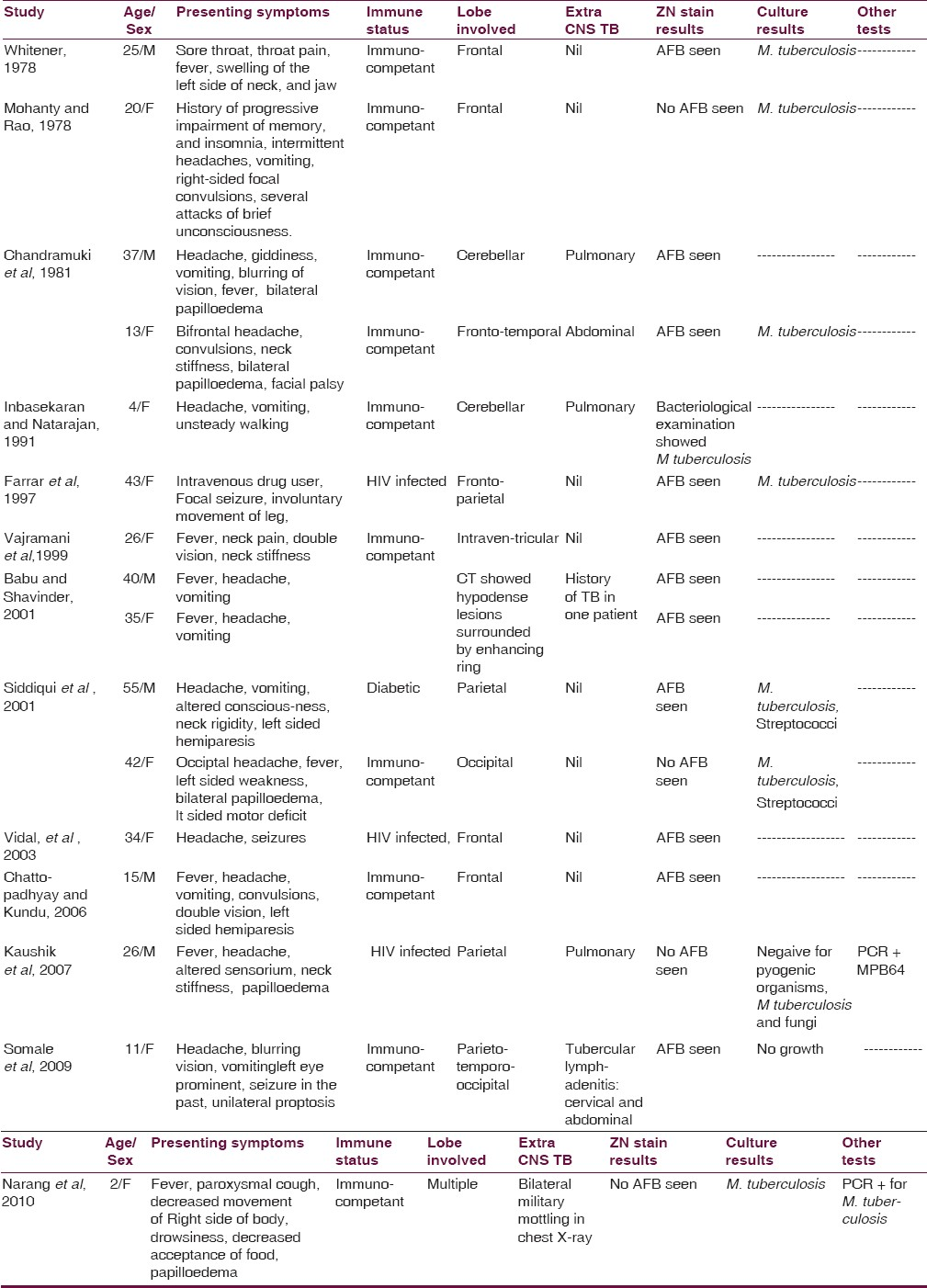
In the present study, the coexistence of pulmonary tuberculosis was seen in two patients. CNS tuberculosis occurs secondary to hematogenous spread of M. tuberculosis from pulmonary Koch's.[15]
Among the laboratory diagnostic modalities used, ZN stain and culture were found to detect the presence of AFB in all the four cases. Table 1 shows that three of the pus specimens grew M. tuberculosis as sole isolate. The fourth case was of concomitant tuberculous and pyogenic brain abscess. A second concomitant pathogen with TBA is rare.[21] There are very few reports of concomitant tuberculous and pyogenic brain abscess that appeared in the literature, namely dual infection due to Streptococci,[12] Toxoplasma,[21] and Echinococcus.[22]
TBAs are an unusual clinical presentation of central nervous system tuberculosis occurring extremely infrequently in developed countries, and almost always in immunocompromised patients. TBA is an uncommon clinical entity, even in countries where tuberculosis is endemic.[23] It occurs in only 4 to 8% of patients with CNS TB who do not have HIV infection[1] but in 20% of patients who do have HIV infection.[2425] We encountered one such case which yielded a pure growth of M. tuberculosis. Fischl et al[21] described a case of TBA and toxoplasma encephalitis in a Haitian woman with AIDS. Farrar et al. reported TBA in a 43-year-old man with a history of intravenous drug use. Vidal et al[13] (2003) reported a case of TBA in a patient with AIDS. They also reviewed the literature from 1981 to 2002 and found eight cases of TBAs in HIV infected patients. Kaushik et al.[15] also reported TBA in a 26-year-old male who was HIV seropositive.
Of these four patients, from the present study, patient no. 1 died who also had an altered level of consciousness at the time of admission. He also gave history of fall but no history of extra CNS tuberculosis. Rest three patients were put on anti-Koch's treatment and being followed up regularly.
Authors appreciate the help of Mr.Moombasawallah, Ms.Nutan and Ms Sonali, RSIC, IIT, Powai, Mumbai for obtaining the NMR spectra.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Pyogenic brain abscess: Findings from in vivo 1.5-T and 11.7T in vitro proton MR spectroscopy. AJNR Am J Neuroradiol. 2005;26:279-88.
- [Google Scholar]
- Proton MR Spectroscopy: Clinical applications. 2002. The Journal of Imaging Technology Management. Available from: http://www.imagingeconomics.com/issues/articles/2002-08_04.asp
- [Google Scholar]
- Tuberculous brain abscess in a patient with HIV infection: Case report and review. Am J Med. 1997;102:297-301.
- [Google Scholar]
- Concomitant tuberculous and pyogenic tuberculous brain abscess. Int J Tuberc Lung Dis. 2001;5:100-1.
- [Google Scholar]
- Tuberculous brain abscess in a patient with AIDS: Case report and literature review. Rev Inst Med Trop Sao Paulo. 2003;45:111-4.
- [Google Scholar]
- Tuberculosis of brain abscess. A diagnostic and therapeutic challenge. J Assoc Physicians India. 2006;54:829-30.
- [Google Scholar]
- Tuberculous brain abscess in a patient with HIV infection. Indian J Tuberc. 2007;54:196-8.
- [Google Scholar]
- Tubercular abscess presenting as unilateral proptosis –A diagnostic challenge. Bombay Hosp J (Special issue):41-4.
- [Google Scholar]
- Multiple intracranial tubercular abscesses in a child. Kathmandu Univ Med J. 2010;8:244-6.
- [Google Scholar]
- Differentiation of tuberculous from pyogenic brain abscesses with in vivo Proton MR Spectroscopy and magnetization transfer MR imaging. Am J Neuroradiol. 2001;22:1503-9.
- [Google Scholar]
- Multimodal Diagnostic Approach to Brain Abscess? 2007. Internet J Trop Med. 3 Available from: http://www.ispub.com/ostia/index.php?xmlFilePath=journals/ijtm/vol3n2/brain.xml
- [Google Scholar]
- Tuberculous brain abscess and toxoplasma encephalitis in a patient with the Acquired Immuno Deficiency Syndrome. JAMA. 1985;253:3428-30.
- [Google Scholar]
- Two cases of cerebral abscess of unusual nature, tuberculous brain abscess and suppurative hydatid cyst. J Neurosurg. 1980;15:572-5.
- [Google Scholar]
- Multiple tuberculous brain abscesses in an HIV-infected patient successfully treated with HAART and antituberculous treatment. Infection. 2003;31:118-20.
- [Google Scholar]
- Infection of the central nervous system by Mycobacterium tuberculosis in patients infected with human immunodeficiency virus (the new neurotuberculosis) Infection. 1999;27:313-7.
- [Google Scholar]
- Tuberculous Brain Abscesses in Immunocompetent Patients: Management and Outcome. Neurosurgery. 2010;67:1081-7.
- [Google Scholar]






