Translate this page into:
Rare complication: Acute syringomyelia due to tuberculoma and tubercular meningitis
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Sir,
A 52-year-old immunocompetent lady was admitted with the complaints of gradual onset progressive altered sensorium with restlessness associated with a history of headache since 3 days. The patient was recently diagnosed as a case of multiple cerebellar and right occipital tuberculoma 2 weeks ago and had been on antitubercular treatment with Isoniazid + Rifampicin (300 mg + 600 mg), PZA 1.5 g, Ethambutol 1 g, and Wysolone 60 mg since then. The diagnosis was confirmed by an MRI brain [Figure 1] which showed cerebellar and right frontal tuberculomas and by CSF examination which showed glucose 13, protein 161, cells 300 with 98% lymphocytes. CSF ADA was high at 24. CSF PCR for TB was positive and an MRI spine screen revealed only degenerative changes in the cervical spine initially. On clinical evaluation, the patient was hemodynamically stable but drowsy and disoriented. Cranial nerve examination revealed left lateral rectus palsy. There was no ptosis or facial deviation and pupils were equal and reacting to light. There was slight hypotonia on the left half of the body. Babinski was positive on the left side. The sensory system could not be assessed. On the 10th day of admission, patient's level of consciousness rapidly deteriorated and hence was shifted to ICU where she was put on a mechanical ventilator. She developed quadriparesis, and had increased tone in the lower limbs along with respiratory failure and bladder dysfunction. Sensory loss could not be assessed at that time. An MRI brain did not show any fresh change but an MRI spine showed syrinx extending from C5 to D6 [Figures 2–7]. It was decided to continue conservative treatment with ATT and steroids. On it, the patient showed gradual improvement.

- Ring enhancing lesion seen in left cerebellum on T1 weighted contrast enhanced gradient echo images.

- T2 W saggital image of the spine showing syrinx extending from C5 up to D6 with extensive degenerative changes in the cervical vertebrae (On the 10th day of admission)
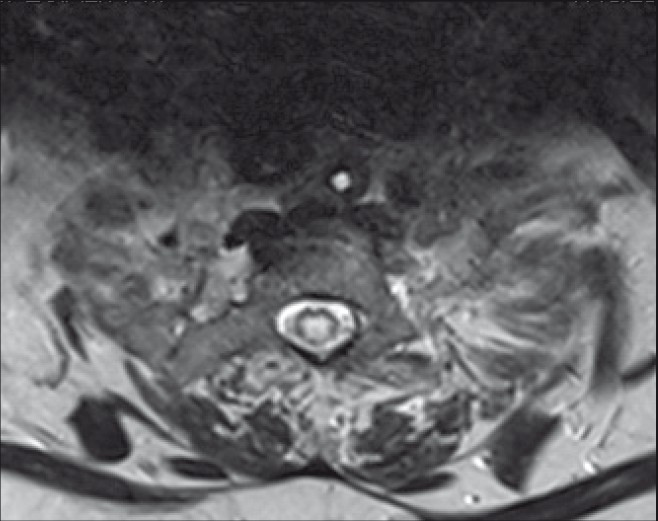
- Axial T2W image showing evidence of central hyperdensity in the spinal cord – Syrinx (On the 10th day of admission)

- T2 W saggital image of the spine showing syrinx extending up to D6 with extensive degenerative changes in the cervical vertebrae (On the 10th of admission)

- T1W saggital image showing evidence of central hypodensity in the thoracic cord suggestive of syrinx

- T2 W saggital image of the spine showing syrinx extending up to D6 with extensive degenerative changes in the cervical vertebrae (On the 10th of admission)
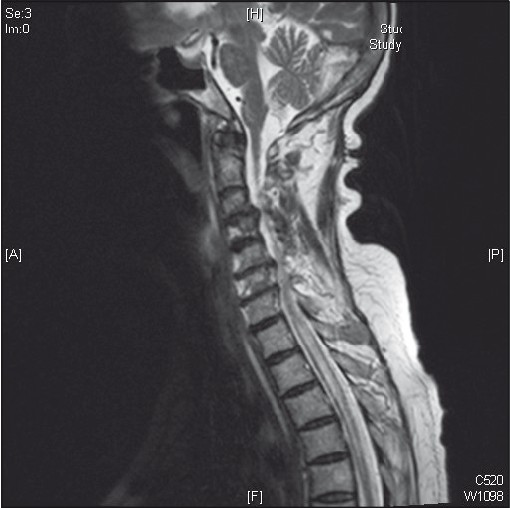
- T2 W saggital image of the spine showing syrinx extending from C5 up to D6 with extensive degenerative changes in the cervical vertebrae (On the 10th day of admission)
Tubercular meningitis (TBM) is the commonest chronic meningitis in India. Syringomyelia can rarely develop as an acute or chronic complication of TBM. The incidence of CNS TB is related to the prevalence of TB in the community, and it is still the most common type of chronic CNS infection in developing countries, like India. The incidence of intracranial tuberculomas as a complication of TBM varies between 1% and 28%.[12] The most frequent outcome in tuberculoma patients is the resolution of tuberculomas and complete clinical recovery within 12 weeks to 1 year with antitubercular therapy.[3] Many cases have been reported of patients developing tuberculomas post-TBM but the development of syringomyelia following TBM is very rare. TBM may rarely be followed by the development of a syrinx even after apparently successful chemotherapy. No medical treatment is known for patients with syringomyelia following TBM. However, a chronic, stable clinical course is common. Surgical treatment most likely will be necessary[45] though ideal treatment of syrinx following TBM is not known. However, our patient has been doing well on ATT without surgery. There has not been any progress of weakness and the condition of the patient remains stable. Thus, though rare acute or chronic syringomyelia can present as a complication of TBM or tuberculoma.
References
- Clinical and radiological features of symptomatic central nervous system tuberculomas. Eur J Neurol. 2005;12:797-804.
- [Google Scholar]
- Syringomyelia: current concepts in pathogenesis, diagnosis, and treatment. J Vet Intern Med. 2006;20:469-79.
- [Google Scholar]





