Translate this page into:
Paraspinal gossybipoma: A case report and review of the literature
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spinal or paraspinal retained surgical sponges (gossybipoma or textiloma) are rare incidents and mostly asymptomatic in chronic cases, but can be confused with other masses such as a hematoma, an abscess or a tumor. In chronic cases, the presentation can be as late as decades after the initial surgery; however, some gossybipomas cause infection or abscess formation in the early stages. The authors report a 40-year-old woman with a history of operation for lumbar disk herniation before 8 months, and got admitted with a complaint of serous fluid leakage from the operation wound. In this report, the authors discuss the clinical presentation, the radiologic findings and the differential diagnosis of gossybipoma.
Keywords
Gossybipoma
retained surgical sponge
spine
surgery
textiloma
Introduction
Although rare, retained surgical sponges can be found subsequently after neurosurgical operations. While the term “textiloma” is used to describe a mass lesion consisting of surgical sponge, the term “gossybipoma” is reserved for both the mass of sponge and the foreign body reaction around it.[12] These pathologies can mimic other common spinal mass lesions such as hematoma, abscess, soft tissue tumor, etc. Their presentation is well known but varies with each case due to different kinds of reactions of body. In literature, 46 cases of gossybipoma involving the spine have been reported;[134–19] however, it is thought to be more than this number because of medico-legal issues. In this report, we present a case of paravertebral gossybipoma, with a short review of the clinical presentation, radiologic findings and differential diagnosis of these lesions.
Case Report
A 40-year-old woman presented with a history of spinal operation for L4–L5 lumbar disk herniation before 8 months and got admitted with non-purulent serous leakage from a small (5 mm) detachment in the surgical wound. The neurologic examination was normal. The wound was minimal erythematous at the detachment site, but there was no tenderness, swelling or fluctuation. There was no fever, and routine laboratory tests including complete blood count, erythrocyte sedimentation rate, c-reactive protein and blood biochemistry were all normal. Microbiologic investigations of the serous leakage revealed no pathogens. While waiting for the microbiological results, treatment with first-generation cephalosporin was started and continued for 4 days, and the serous leakage stopped immediately with secondary healing of the wound in a 1-week period. However, the patient's same complaints recurred, and thus she got admitted again to our clinic. A computed tomography (CT) of the lumbar vertebrae revealed a hyperdense mass lesion located in the left side of the previous operation site. Magnetic resonance imaging (MRI) showed a mass lesion in the left paravertebral area, which was hypointense on T1- and T2-weighted images, with peripheral hyperintense ring in T2-weighted images. MRI post-contrast images showed ring enhancement of the lesion [Figure 1]. CT-guided biopsy was performed but no materials were obtained.
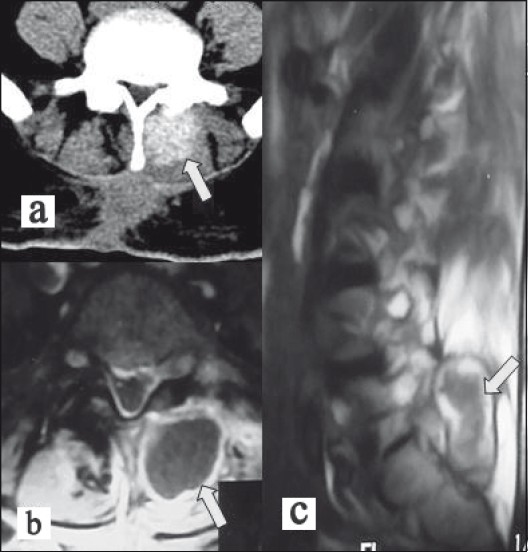
- Lumbar imaging of our case revealed a paravertebral mass lesion located in the left side of the previous operation site (arrows). (a) Axial CT scan, (b) axial post-contrast enhanced MRI, (c) sagittal T2-weighted MRI
The patient was operated by lumbar midline reincision, and the exploration of the left paravertebral area revealed a retained sponge. The sponge was found adherent to the surrounding soft tissue by the new formed fibrotic tissue, which required individual dissection of these fibrotic attachments. No concomitant abscess was found. The lesion was removed with no intraoperative complications. Histopathologic examination revealed mononuclear cell infiltration and fibrosis formation around the retained sponge [Figure 2]. Postoperatively, treatment with first-generation cephalosporin was continued. The patient's complaints showed improvement with no neurologic deficits, and the patient was discharged on postoperative day 3 without complications.
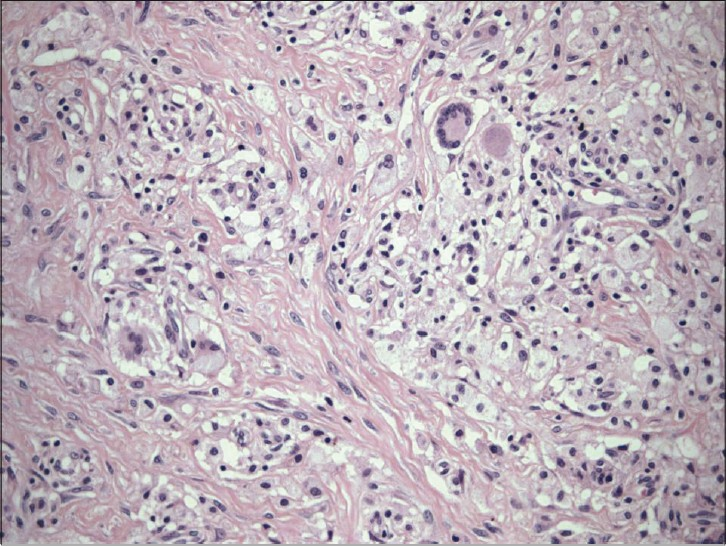
- A photomicrograph shows the mononuclear cell infi ltration and fi brosis formation around the retained sponge (H and E, ×200)
Discussion
Many different kinds of hemostatic agents – absorbable and non-absorbable – are used to control intraoperative bleeding in neurosurgical operations. Non-absorbable materials include various forms of cotton pledgets and synthetic hemostats, which should be removed before surgical closure.[20]
Retained surgical sponges can be found following abdominal, gynecologic, urologic, thoracic, orthopedic or neurosurgical procedures. They are encountered in abdominal and thoracic cavities more commonly but they are also reported after extremity and spinal surgeries. Retained sponges are more common in obese patients and after emergency surgery.[15] A retained surgical sponge is thought to be a common entity; however, due to the medico-legal issues, only a few cases in the literature have been reported. The reported incidence of these lesions varies between 1/1000 and 1/10,000.[21]
While the term “textiloma” is used to describe a mass lesion consisting of surgical sponge, the term “gossybipoma” is reserved for both the mass of sponge and the foreign body reaction around it.[12] In the literature, there are 46 reported cases of gossybipoma after spinal surgery since 1965.[134–19] In these reports, patients had presented mostly with complaints of back pain, common motor weakness and/or sensory deficits in neurologic examination, with no infectious findings, at which the placement of surgical sponge occurred at least a couple years ago before the admission.[1517–19] On the other hand, some cases admitted with fluid leakage after only a short time of the first operation.[22] In our case, the patient presented with sterile serous leakage from the operation wound, 8 months after the previous operation.
After surgery, the body gives two types of foreign body reactions against retained sponges: (1) the exudative type tissue reaction, which leads to acute abscess formation, with a tendency to form fistulas through the skin and (2) aseptic fibrous tissue reaction, which involves slow adhesion formation, such as encapsulation and granuloma formation.[5] While the time interval to clinical presentation is short with the exudative type tissue reaction, it ranges to even decades after surgery with aseptic fibrous tissue reaction.[11]
Surgical sponges with radiopaque markers are used now in most of the medical centers. Due to this imaging characteristic of the gossybipomas, plain radiographs and/or CT scan can be useful in cases suspected with these lesions. However, gossybipomas may not be easily recognized even on CT scans.[23] Kopka et al.[24] had reported 13 patients with gossybipomas in thorax and abdomen, and remarked that the radiopaque marker inside the gossybipoma was seen in only nine patients (69.2%) and even then did not always lead to diagnosis. In our case, the gossybipoma was revealed in CT scans as a hyperdense mass lesion, although it was not diagnostic for this lesion.
Because the differential diagnosis of paraspinal lesions in patients with history of spinal operations include hematomas, abscess or residual/recurrent tumors, MRI with intravenous contrast enhancement is known to be the best radiologic investigation modality in these situations [Table 1]. Kim et al.[5] stated that MRI usually shows a well-defined mass with a fibrous capsule that exhibits low signal intensity on T1-weighted images compared with the signal intensity of the paravertebral back muscles, high signal intensity in the center with hypointense rim on T2-weighted images, and strong peripheral enhancement in post-contrast images. On the other hand, MRI of our case demonstrated a mass lesion, which was hypointense on both T1- and T2-weighted images, with peripheral hyperintense ring in T2-weighted images and peripheral enhancement in post-contrast images. These findings were different from what had been stated in previous reports.[51025] Accordingly, we believe that despite the importance of the MRI in the diagnosis of gossybipoma lesions, the definitive diagnosis must be mainly aided by the high suspicion profile of the physician and the intraoperative findings.

Conclusion
In patients with the history of spinal operation, gossybipomas should always have a place in the differential diagnosis of newly found lesions, as it is believed that they are much more common than they are reported. MRI is the best radiologic modality for the diagnosis. However, no pathognomic radiologic characteristics are defined for these lesions. For this reason, the definitive diagnosis must be mainly aided by the high suspicion profile of the physician and the intraoperative findings. Moreover, gossybipomas are rare, but possible to occur. Thus, it must be remembered that careful inspection of the surgical field before closure is still an important basic rule in surgery.
Source of Support: Nil,
Conflict of Interest: None declared.
References
- Gossypiboma: the problem of the retained surgical sponge. Radiology. 1978;129:323-6.
- [Google Scholar]
- CT appearance of a surgically retained towel (gossypiboma) J Comput Assist Tomogr. 1986;10:343-5.
- [Google Scholar]
- Retained surgical swab debris in postlaminectomy arachnoiditis and peridural fibrosis. J Bone Joint Surg Br. 1998;70(B):659-62.
- [Google Scholar]
- Retained surgical sponge in differential diagnosis of paraspinal soft-tissue mass after posterior spinal surgery: report of eight cases. Neurol India. 2009;57:320-3.
- [Google Scholar]
- MR imaging findings of paravertebral gossypiboma. AJNR Am J Neuroradiol. 2007;28:709-13.
- [Google Scholar]
- MR and CT imaging of paraspinal textiloma (gossypiboma) J Comput Assist Tomogr. 2001;15:1000-3.
- [Google Scholar]
- MRI features of neurosurgical gossypiboma: report of two cases. Neuroradiology. 1996;38:468-9.
- [Google Scholar]
- Uncommon intraspinal space occupying lesion (foreignbodygranuloma) in the lumbosacral region. Neuroradiology. 1985;27:354-6.
- [Google Scholar]
- Identification of a retained surgical sponge using magnetic resonance imaging. Neurosurgery. 1986;18:496-8.
- [Google Scholar]
- Retained surgical sponge 40 years after laminectomy: case report. Surg Neurol. 1988;30:235-6.
- [Google Scholar]
- Suture granuloma mimicking a lumbar disc recurrence: case illustration. J Neurosurg. 1997;87:473.
- [Google Scholar]
- Foreign body granuloma simulating solid neoplasm on MR. Clin Imaging. 1997;21:269-72.
- [Google Scholar]
- Foreign body granuloma mimicking a benign intra spinal tumor. Br J Neurosurg. 1999;13:417-9.
- [Google Scholar]
- Sponge Induced Granuloma (“Gauzoma“) as a Complication of Posterior Lumbar Surgery. Neurol Med Chir (Tokyo). 2005;45:209-11.
- [Google Scholar]
- Textiloma: a case of foreign body mimicking a spinal mass. Eur Spine J. 2006;15:626-9.
- [Google Scholar]
- A retained surgical sponge (gossypiboma) mimicking a paraspinal abscess. Br J Neurosurg. 2007;21:307-8.
- [Google Scholar]
- A 13-year-old textiloma (gossypiboma) after discectomy for lumbar disc herniation: a case report and review of the literature. Spine J. 2007;7:618-21.
- [Google Scholar]
- Textiloma (gossypiboma) mimicking recurrent intracranial tumor. Arch Pathol Lab. 2004;128:749-58.
- [Google Scholar]
- Retained surgical sponges, a denied neurosurgical reality. Cautionary note? Neurosurg Rev. 2007;24:41-3.
- [Google Scholar]
- Ultrasonography and x-ray computed tomography in the diagnosis of intraabdominal textiloma. Apropos of 12 cases. J Radiol. 1988;69:243-51.
- [Google Scholar]
- CT of retained surgical sponges (textilomas): pitfalls in detection and evaluation. J Comput Assist Tomogr. 1996;20:919-23.
- [Google Scholar]
- Magnetic resonance imaging of retained surgical sponge. Case report. Clin Imaging. 1992;16:259-62.
- [Google Scholar]






