Translate this page into:
Spectrum of surgical trauma and associated head injuries at a university hospital in eastern Nepal
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Trauma is one of the common surgical emergencies presenting at B. P. Koirala Institute of Health Sciences (BPKIHS), Nepal, a tertiary referral center catering to the needs of the population of Eastern Nepal and nearby districts of India.
Objective:
The objective of this study is to analyze the magnitude, epidemiological, clinical profile and outcome of trauma at B P Koirala Institute of Health Sciences.
Materials and Methods:
This descriptive case series study includes all patients with history of trauma coming to BPKIHS emergency and referred to the surgery department. We noted the detailed clinical history and examination, demographics, mechanism of injury, nature of injury, time of reporting in emergency, treatment offered (operative or non operative management) and analyzed details of operative procedure (i.e. laparotomy, thoracotomy, craniotomy etc.), average length of hospital stay, morbidity and outcome (according to Glasgow outcome scale). Collected data were analyzed using EpiInfo 2000 statistical software.
Results:
There were 1848 patients eligible to be included in the study. The mean age of the patients was 28.9 ± 19.3 years. Majority of the patients (38%) belonged to the age group of 21 - 40 years and the male to female ratio was 2.7:1. Most of the trauma victims were students (30%) followed by laborers (27%) and farmers (22%) respectively. The commonest causes of injury were fall from height (39%), road traffic accident (38%) and physical assault (18%); 78% of the patients were managed conservatively and 22% underwent operative management. Postoperative complications were seen in 18%. Wound infection 7.5%, neurological deficit including cerebrospinal fluid (CSF) otrorrhea was seen in 2.2% patients. Good recovery was seen in 84%, moderate disability in 5.2% patients and severe disability in 1.4% patients. The mortally was 6.3% and most of the deaths were related to traumatic brain injuries.
Conclusions:
In Nepal, trauma-related injury contributes significantly to morbidity and mortality and is the third leading cause of death. There are very few studies on trauma from this country and hence this study will help in understanding the etiology and outcome particularly in the Eastern region of Nepal.
Keywords
Craniotomy
laparatomy
trauma
Introduction
Injury has been man's constant companion since the earliest time, however, despite its huge importance, trauma has been called the neglected disease of modern society.[1] Trauma or injury has been defined as damage to the body caused by an exchange with environmental energy that is beyond the body's resilience.[2] The first recorded account of injuries is in the Edwin Smith Papyrus (written over 5000 years ago) gives an account of 48 different types of injuries with an approach to the wounded individual. Trauma remains one of the leading causes of death and disability in both industrialized and developing countries and globally, it is the seventh leading cause of death.[3] In Nepal, trauma or injury contributed to 9% of total mortality and is the third leading cause of death.[4] This study has been undertaken to help understand the etiology and outcome of traumatic injuries in the Eastern region of Nepal.
Materials and Methods
This is a prospective descriptive study conducted at the Department of Surgery, (BPKIHS) from March 15, 2006, to March 14, 2007. All patients with history of trauma coming to the emergency were included in the study, except those with isolated musculoskeletal, eye, ear, nose, throat injuries. Relevant investigations like hHemoglobin, total leukocyte count (TLC), differential count (DLC), blood sugar and urea, serum creatinine, serum electrolytes, blood grouping, arterial blood gas (ABG), ECG, X-ray chest, X-ray abdomen, X-ray spine, X-ray pelvis, ultrasonography of abdomen and pelvis and computerized Tomography (CT) head were done as and when indicated. Patients with minor injuries were discharged after adequate treatment and the rest were further evaluated in detail by the surgical team under the supervision of consultant on duty and the indications for operative or non operative management decided upon. Epidemiological factors like the magnitude of the problem, clinical profile, demographics, mechanism and mode of injury, time of presentation since the injury, details of injuries according to relevant organ or system, management details (conservative or operative) were assessed. The average length of hospital stay, morbidity (wound infection, burst abdomen, organ specific complication) and postoperative outcome, including Glasgow Outcome Score (GOS) were measured and data was analyzed in Microsoft excel ((Microsoft Corporation, Redmond, WA) using Epi Info Version 3.5.1 (Atlanta, GA: Centers for Disease Control and Prevention) statistical software.
Results
During the period of study, a total 6793 patients attended the emergency department, 1848 (27.2%) were referred to the Department of Surgery for the evaluation. Out of these 1144 cases (61%) were admitted as inpatients, 704 cases were managed as outpatient, the commonest injury was bruise / abrasion in 366, followed by superficial laceration in 268 and minor injuries including sprains/nonspecific complaints and headache and were discharged from emergency after adequate primary treatment. The mean age of the patients was 28.9 ± 19.3 years (range 0.33-96 years) with majority of the patients [704 (38%)] belonging to the 21-40 year group [Figure 1]. The male to female ratio was 2.7:1 (1354 and 494 respectively). The mean duration of presentation since the incident was 19.8 hours (range of 0.08-338). Majority of the trauma patients sustained injuries either on the highways, street (43%) with an equal number sustaining injury at home (43%) [Figure 2]. Other places of injuries were work place, school, recreational place, mountains and blast injury (14%) [Figure 3]. Students were the most common patients (52%) followed by laborers (34%) and then farmers (14%). The mean time of presentation after injury was 19.8 ± 35.5 hours. The earliest presentation was at 15 minutes with one case presenting a month after the injury.
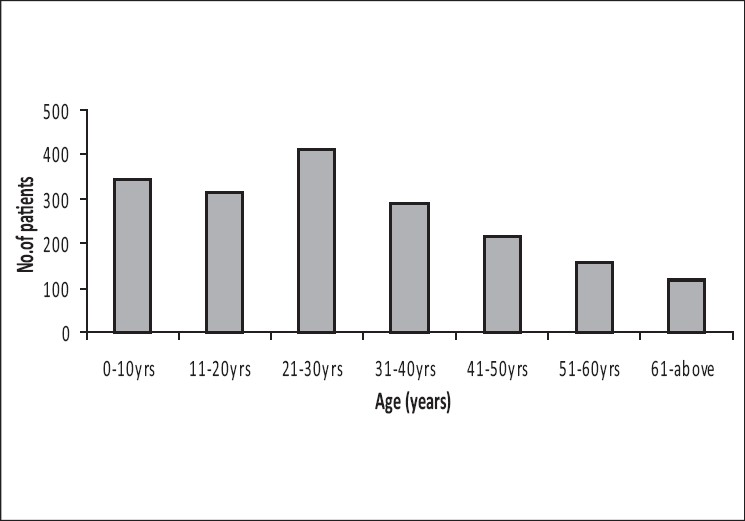
- Age group distribution
- Mode of injury
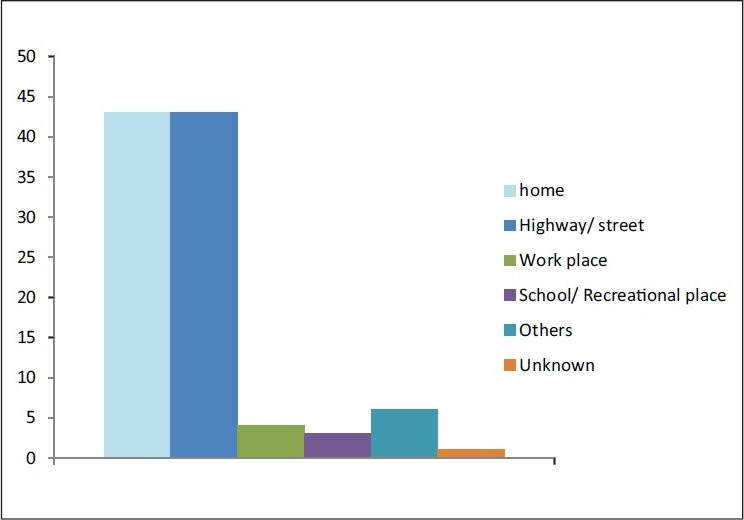
- Place of injury
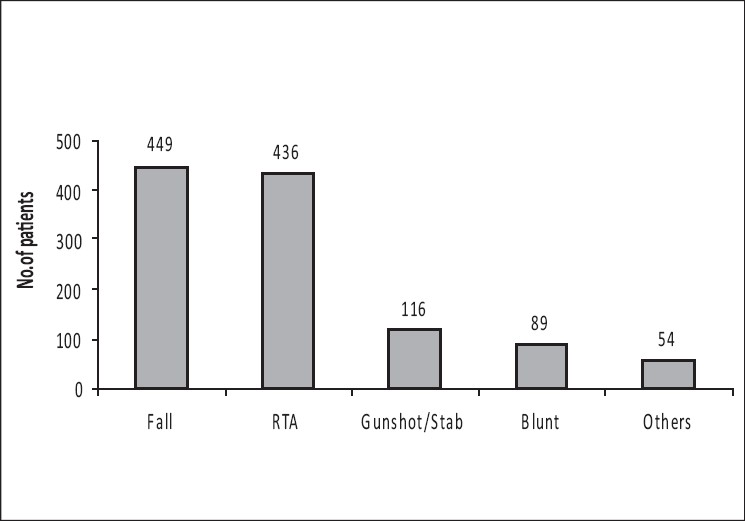
Majority of the patients were transported by local ambulance to the hospital and a few of them by other motor vehicles, animal carts and even by bicycles. The commonest mode of injury was secondary to fall (39%) followed by road traffic accident (38%). Of the cases with RTA the majority (60%) were hit-and-run victims found on the road, with the rest comprising vehicle occupants (10%) and pedestrians hit by a vehicle (30%). Eighteen per cent of the patients suffered physical assault with the majority suffering from penetrating (stab/gunshot) injury (51%) followed by blunt trauma (44%) and the rest 5% sustaining injuries by bull/ buffalo, crush by machine, animal bite, sickle injury and bomb blast. With respect to the site of injury, the most common site was the head in 733 cases followed by the abdomen in 204 cases, face and neck in 60 cases and chest in 176 cases. There were 43 cases with multiple site injury. Most incised and lacerated wounds were encountered in head including face and scalp region, whereas fractures predominantly involved the upper limbs [Figure 4]. The commonest symptom was loss of consciousness, present in 44%, followed by vomiting (33.7%), headache (16.7%) and seizure (1.5%). Pain chest and abdomen was present 20% and 10% respectively. Eight per cent of the patients were under the influence of alcohol at the time of sustaining injury and presentation.
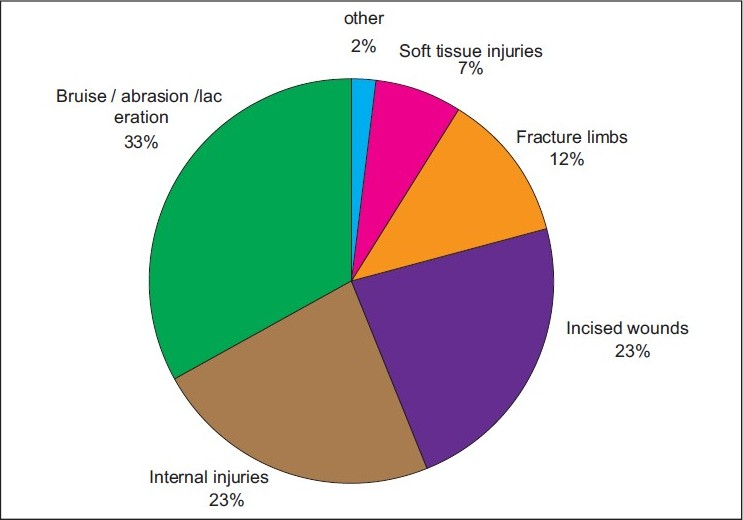
- Organ specific site of injury
Traumatic brain injuries
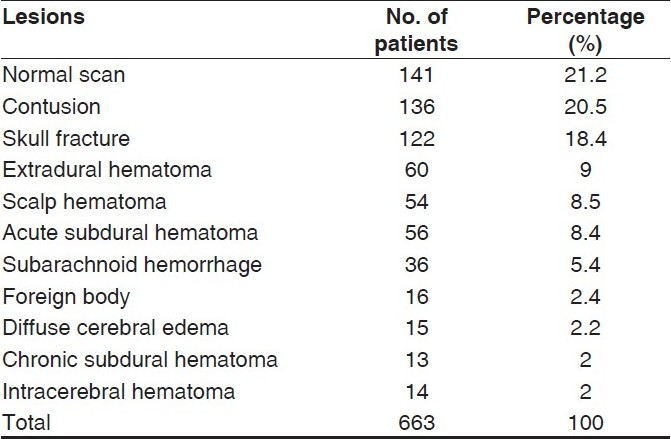
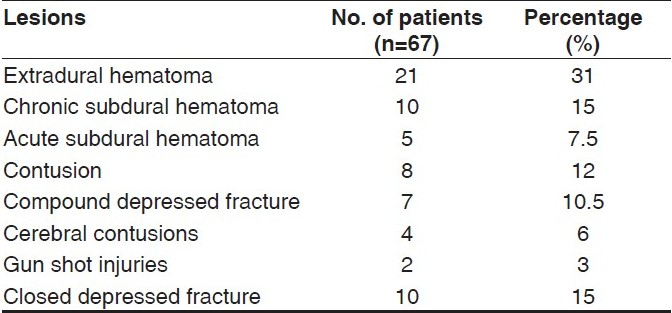
Most of the traumatic brain injury cases were due to RTA (358 cases), followed by fall (287 cases) and physical assault (62 cases). The others were due to gun-shot in 16 cases and blunt trauma in 10. On GCS examination, majority of the head injuries were in the mild category (553 cases) followed by severe head injury in 115 cases and moderate in 65 cases. Of the total of 733 cases with head injury, only 663 required CT scan. The CT was abnormal in 491 of the 663 cases (77.5%). CT showed contusion in 136 cases, fracture skull in 122 cases, epidural hematoma in 60 cases, scalp hematoma in 54 and acute subdural hematoma in 56 cases [Table 1]. There were also 36 cases of traumatic subarachnoid hemorrhage, 14 cases of intracerebral hematoma and 13 of chronic subdural hematoma. Of the 733 cases with traumatic brain injury (TBI), only 87 were operated (11.8%). The commonest neurosurgical procedure was evacuation of epidural hematoma in 29 cases, depressed fracture elevation in 20 cases, contusectomy in 12 and chronic subdural hematoma evacuation in 10 cases [Table 2]. The rest were 14 cases of acute subdural and two gun-shot injuries.
Thoracic injuries
Radiological examination showed isolated abnormal chest X-ray in 172 patients (15%). Majority of the cases were secondary to fall (76), RTA (54), assault (18), gunshot injury in 14 and bull gore injury in the rest (10 cases). Blunt chest trauma was present in 118 cases, penetrating in only 34 cases and 20 cases were associated with other injuries. Abnormalities seen on chest X-ray were hemothorax in 28 cases, pneumothorax in 14 cases, pneumoperitoneum in 26 cases, fracture ribs alone in 88 cases and fracture ribs with hemothorax or flail chest in 10 and six cases respectively. The most common cause of chest injury was fall followed by RTA in the blunt group and gunshot followed by assault in the penetrating group. Of these, 62 cases (36%) underwent intercostal chest tube drainage for hemothorax /pneumothorax or a combination of both.
Abdominal injury
There were a total of 204 cases (17.7%) with abdominal trauma. The majority of abdominal injury cases were secondary to fall (97 cases), followed by RTA (40 cases), assault (31) and 14 cases each of gunshot and suicidal attempt. There were eight cases with bull gore injury. Blunt injury was present in 133 cases and penetrating in 71 cases. Abdominal ultrasound was done in 156 patients (13.6%) cases where the index of suspicion of injury was high or in doubt. Of the 156 cases, 42 patients (26.9%) showed normal scan, 44 (28.2%) had hemoperitoneum, 39 (25%) showed collection in peritoneal cavity, 17 (10.8%) had splenic laceration and 14 (8.9%) had liver contusion. There were 70 surgical procedures, of these, 56 were for gastrointestinal tract perforation and 14 for solid organ injury. Gastrointestinal tract injury was present in 56 cases with ileal perforation being the commonest (39.2%), followed by jejunum (21.4%) and stomach (21.4%). The rest had injuries to the duodenum (7%), colon (7%) and rectum in two cases (4%). The commonest surgical procedure done in the gastrointestinal tract group was resection anastomosis in 14 cases, followed by primary closure for injury of the ileum (8 cases), stomach (12) and jejunum (12). There were four cases each of duodenal injury with gastrojejunostomy and colostomy for colonic perforation. Splenectomy was done in four cases and splenic packing in two. There were two nephrectomies and two cases of primary repair of renal laceration. Of the four cases with bladder perforation, two each of extra and intraperitoneal repair of bladder was performed.
Outcome
There were 72/1144 mortality (52 secondary to head injury, 18 secondary to abdominal injury and two due to chest trauma). The overall mortality rate was 6.29%. Out of 733 neurosurgical patients there were 52 deaths. Good recovery was seen in majority of the cases (80%), moderate disability in (12%) patients and severe disability in 54 (8%). Postoperative morbidity was seen in 44/1144 patients (3.8%). The commonest cause was wound infection in 24 cases, permanent neurological deficits in 16 and aspiration pneumonia with chronic chest infection in four patients. All four with chest infection had also burst abdomen.
Discussion
Data on trauma differ from one center to another because of geographic and economic patterns of a country, education, poverty, political and religious practice.[7] A few studies on RTA have been conducted in Nepal but, to the best of our knowledge, this is the first one in this country studying the overall epidemiological profile of trauma and its outcome in detail.[48] The common age of presentation was the second and third decade which is similar to the many other studies.[4–6] The male preponderance in our study reflects that the greater mobility of males for either work, recreation or for other activities such as males are more likely to be employed as drivers and mechanics in cars and trucks resulting in a higher exposure to the risk of traffic injuries.[101139] The mean duration of presentation since the incident in this study was 19.8 hours. In a study by Henderson et al. in the United Kingdom, the median time for operation for abdominal trauma since the emergency call was 127 minutes.[12] In a study by Grossman et al. in 669 crashes, the median interval between crash and emergency medical services (EMS) dispatch was five minutes, the median scene time was 15 minutes, and the median interval between dispatch and emergency department arrival was 48 minutes.[13] The time to arrival to the hospital is significantly higher in present study and attributable to the lack of transportation, which is poor in developing countries, apart from this many of our patients were from the mountains and hilly areas where roads are absent.[3] RTA was one of the major causes of trauma in this study, which is in accordance with other studies which have shown it still remains the major cause of injury in the developing world.[14–1638–404243] The high incidence of fall injury in this study is partly attributable to the hilly and mountainous geography of the country where collecting fodder from the forest is a common mode of living for many. Common indications for CT scan are loss of consciousness, vomiting and headache.[17] CT scanning has been usually reserved for patients considered to be at high risk of intracranial complication and medico legal consideration.[18] In our series, the threshold for ordering CT scan was kept low because of the difficulty in accessing the hospital once discharged, for medico legal reasons and also because of the low probability of follow up. This gave a positive CT finding in 79% patients.
A normal CT scan, although ruling out major intracranial pathology, will not rule out diffuse axonal injury which can result in either obvious neurological sequelae or more subtle signs and symptoms.[19–21] In this study, TBI secondary to RTA was present in 64% which is similar to other studies from Asia and developed countries.[22232526] Majority (60%) of the cases with RTA were hit-and-run victims, 42 (10%) were vehicle occupants and 135 (30%) were pedestrians hit by a vehicle. The high pedestrian rate is similar to other studies with a range of between 28-48%.[283940] These results contrast with the study from Greece, which showed that in 730 consecutive patients with RTA, 444 were motorcyclists (60.8%), 209 were car occupants (28.7%), and only 77 were pedestrians (10.5%).[24] The major involvement of pedestrians (30%) as victims to RTA could be attributed to the lack of public awareness of road safety, outdated vehicles, non implementation of traffic laws, and lack of adequate sidewalks and unhindered encroachment of available sidewalks by vendors and buildings- which is a common sight in any developing country in the world.[3840] The high rate of hit-and-run victims partly reflects the poor traffic laws and action in this country, where there are no electronic speed control checks or cameras to monitor the roads which have been shown to reduce intersection crashes by 25-40%.[47]
In a similar study from Asia, the Malaysian National Trauma Database studied the profile of trauma from five tertiary referral centers for one year (2005-6) where from a total case of 123,916, RTA accounted for 72.6% of injuries with 64.9% involving motorcyclist and pillion rider.[23] Similarly from a study from New Zealand, from a total of 160 cases of motor vehicle accidents, head injury was present in over 60% of all patients. Vehicle occupants comprised 51% of the group, pedestrians 28% and motorcyclists 21%.[28]
Fifteen per cent cases in this study had chest injury. The number is significantly higher when compared with the study from UK, which had only 29 cases in a three-year period.[29] The major cause of chest trauma in this study was fall, followed by RTA, with hemothorax / pneumothorax in 24% and fracture ribs in 51%. This is similar to studies from other developing countries. In a study from Iran in 276 chest injuries, RTA was the main cause of injury, especially for pedestrians, followed by stab wound (89 cases, 32.1%) and fall injuries (32 cases, 11.6%), respectively.[30] Hemothorax or pneumothorax (50.4%) and rib fracture (38.6%) were the most common types of chest injury. In another study by Kulshrestha et al. in 1359 chest trauma patients, blunt injury was present in 90.1% and penetrating in 9.9%. Majority of them were secondary to RTA (55.7%) and 20.4% had hemothorax / pneumothorax, 48.7% had rib fractures with 18.3% needing tube thoracostomy.[31] Penetrating chest trauma was present in only 19% in this study with none requiring open thoracotomy which is similar to the three-year study from Edinburgh, where from a total of 120 patients with penetrating chest trauma, only 19% needed one or more tube thoracostomies with 5% undergoing thoracotomy.[29]
Ultrasonography is a rapid, portable, noninvasive, and accurate examination that can be performed in emergency to detect any peritoneal collection or organ injured. In our setup most of the patients come from low socioeconomic strata and can’t afford the expenses of CT scan. We have to thus rely on ultrasonographic finding for the majority of the emergency surgical or non-surgical decisions. Abdominal ultrasound was performed in 156 patients (13.6%), mostly in blunt trauma cases where the index of suspicion of solid injury was high. Thirty two patients (20.5%) showed normal scan while (21.7%) were presented hemoperitoneum, (20.5%) showed collection in peritoneal cavity, and (7.6%) patients had splenic laceration with hemoperitoneum, (5.1%) had liver contusion respectively.
Average organ-specific sensitivity of abdominal USG was 86%. Heindel et al. showed that the most frequent reason for USG consultation in emergency department was acute abdominal pain (70%) and blunt abdominal trauma (70%) patients. Sonography after blunt abdominal trauma was considered appropriate in (90%). Diagnostic information was obtained in (90%), and therapeutic interventions were required in (10%).[34] There were 56 cases with blunt and 14 with penetrating abdominal trauma in this study; the commonest cause again being RTA, as in other studies from this region. A study in India by Dharap and Changlani finds RTA (52%) to be the commonest cause of abdominal trauma followed by fall (28%) and interpersonal violence (20%).[32] In the penetrating injury group, stabbing was responsible for most of the cases. These injuries are similar to some of the studies from the west.[33] Perforation of the bowel was the commonest injury in blunt trauma cases. In a study from Nigeria in 19 children with abdominal trauma, there were a total of 23 injuries with most of the injuries in the jejunum and ileum (10 perforations, two contusions with one mesenteric hematoma and one mesenteric tear). These studies show that the gastrointestinal tract remains the commonest organ of injury in abdominal trauma.[34]
With respect to TBI and its outcome based on GOS, good recovery was present in 545 (80%), moderate disability in 82 (12%) patients and severe disability in 54 (8%). Some studies have shown an increasing death rate from TBI, for example in a study from India, over a period of eight years (1996 to 2003). The traumatic brain injury deaths showed a steady increase in number from year with the majority in the younger age (18.8%) and in males.[48] The mortality rate in this study secondary to TBI was 7% (overall mortality rate was 6.29%) which is similar to most studies and lower than some other.[15162223] This emphasis the importance of proper trauma regionalization and structuring which has statistically shown to reduce the mortality.[49]
Thus trauma remains the leading causes of death claiming about 130,000 lives per year in USA and approximately 17,500 deaths in Mexico during 2000.[44] RTA increased 68-fold between 1951 -1999 (6000-413,000) with the injuries increasing 56-fold (5000-6,000) and fatalities 97-fold (852-84,000) in China, over the same period.[4245] Similarly there has been a fourfold increase in road fatalities over the last 30 years in Kenya.[46] Some studies, though, have shown a reduced incidence of trauma (from 17 deaths per 100,000 population in 1960 to 10 deaths per 100,000 population in 2000).[40]
Conclusion
The incidents of trauma and trauma-related deaths have increased in the last decade. Trauma usually affects the younger generation, which leads to a major social and economic burden in developing countries. There are no comparative studies from Nepal but this study has shown that majority of the trauma cases are due to preventable causes like, improper roads, bad planning of houses, loose traffic laws, not wearing of helmets or seatbelts and by using alcohol during driving. The Government needs to consider these factors into the national health policy so as to reduce the mortality and morbidity from trauma. The need for trauma care systems (regional / local / national) should be the priority for any developing country based on their regional geography and health care systems. Education too plays a major role in the implementation of law and order. Improvement in data collection, research and monitoring will help in better safety of pedestrians, passengers and drivers. This study has limitations that the long term follow-up was not done and neither was the details preceding the trauma in RTA studied. Further research into individual contributing factors can result in decrease in RTA deaths. This should be done with making the public more aware of traffic rules and regulations and imposing stricter fines for defaulters by the policy makers. The transport department must also be involved to improve the roads, lighting, proper speed breakers and maintenance of the road.
Last, but not the least, the health department must actively recruit medical centers on the highways/roads/local or district levels, with training in basic ABC in trauma resuscitation for early intervention and referral to save lives. Incorporating the do and don’t in school curriculum is another method to make children aware of the hazards and complications of trauma.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Injuries and trauma. In: Russell RC, Norman S, Cristopher JK, eds. Bailey and Love's Short Practice of Surgery (24th ed). London: Arnold; 2000. p. :279-91.
- [Google Scholar]
- Trauma. In: Brunicardi F, ed. Schwartz's Principle of Surgery (8th ed). New York: McGraw-Hill; 2005. p. :129-88.
- [Google Scholar]
- Management of Acute Trauma. In: Townsend CM, ed. Sabiston Text book of Surgery (17th ed). Philadelphia: Townsend, Beauchamp, Evers and Mattox; 2005. p. :483-532.
- [Google Scholar]
- Epidemiological study of road traffic accident: A study from eastern Nepal. WHO Regional Health Forum. 2004;8:15-22.
- [Google Scholar]
- Essential Surgical Practice (4th ed). London: Hodder Arnold Publication; 1999. p. :1-42.
- Enhanced trauma program commitment at a level I trauma center: Effect on the process and outcome of care. Arch Surg. 2003;138:838-43.
- [Google Scholar]
- The surgery of urban violence. In: Ellis BW, ed. Hamilton bailey's emergency surgery. (13th ed). K.M. Varghese Company; 2000. p. :110-20.
- [Google Scholar]
- An epidemiological study of road traffic accident cases attending emergency department of teaching hospital. J Nepal Med Assoc. 2006;45:238-43.
- [Google Scholar]
- Blunt and penetrating abdominal injuries: A study of 51 cases. J Postgrad Med. 1983;29:96-9.
- [Google Scholar]
- Road traffic accidents cases at BPKIHS, Dharan, Nepal: One year in retrospect. J Nepal Med Assoc. 1997;35:241-4.
- [Google Scholar]
- Automobile versus pedestrian injuries: Does gender matter? J Emerg Med 2008 in press
- [Google Scholar]
- From roadside to bedside: the regionalization of trauma care in a remote rural county. J Trauma. 1995;38:14-21.
- [Google Scholar]
- Teaching hospital perspective of the quality of trauma care in Lagos, Nigeria. World J Surg. 2001;25:112-5.
- [Google Scholar]
- Epidemiological patterns of head injury in a newly established neurosurgical service: One-year prospective study. Afr J Med Sci. 2008;37:383-8.
- [Google Scholar]
- 3000 head injuries: A prospective study of patients admitted to Brisbane neurosurgical units. J Clin Neurosci. 1998;5:402-5.
- [Google Scholar]
- Emergency department discharge of patients with a negative cranial computed tomography scan after minimal head injury. Ann Surg. 2000;232:126-32.
- [Google Scholar]
- Magnetic resonance imaging finding in severe head injury patients with normal computerized tomography. Turk Neurosurg. 2008;18:1-9.
- [Google Scholar]
- Outcome of patients with diffuse axonal injury: The significance and prognostic value of MRI in the acute phase. J Trauma. 2000;49:1071-5.
- [Google Scholar]
- The structural basis of moderate disability after traumatic brain damage. J Neurol Neurosurg Psychiatry. 2001;71:521-4.
- [Google Scholar]
- Mortality pattern according to autopsy findings among traffic accident victims in Yazd, Iran. Chin J Traumatol. 2008;11:329-34.
- [Google Scholar]
- National Trauma Database (NTrD)--improving trauma care: First year report. Med J Malaysia. 2008;8:45-9.
- [Google Scholar]
- Motor vehicle trauma: Analysis of injury profiles by road-user category. Emerg Med J. 2006;23:27-31.
- [Google Scholar]
- Epidemiology and 12-month outcomes from traumatic brain injury in Australia and New Zealand. J Trauma. 2008;64:854-62.
- [Google Scholar]
- Head injuries in adolescents in Taiwan: A comparison between urban and rural groups. Surg Neurol. 2006;66:14-9.
- [Google Scholar]
- Incidence and severity of head and neck injuries in victims of road traffic crashes: In an economically developed country. Int Emerg Nurs. 2009;17:52-9.
- [Google Scholar]
- Splenic trauma: An Indian experience recent advances in surgery. Jay Bro. 1996;5:235-54.
- [Google Scholar]
- Prospective observation of abdominal ultrasound in radiological emergency services: Approaches to cost saving. Rofo. 2003;175:1207-9.
- [Google Scholar]
- Gastrointestinal injuries following blunt abdominal trauma in children. Niger J Clin Pract. 2008;11:250-3.
- [Google Scholar]
- Preliminary analysis of the care of injured patients in 33 British hospital: First report of the United Kingdom Major trauma outcome study. BMJ. 1992;6:737-40.
- [Google Scholar]
- Reducing accident death rates in children and young adults: The contribution of hospital care, Steering Committee of the Major Trauma Outcome Study Group. BMJ. 1996;313:1239-4137.
- [Google Scholar]
- Pattern of road traffic injuries in Ghana: Implications for control. Inj Control Saf Promot. 2003;10:69-76.
- [Google Scholar]
- Death and injury from motor vehicle crashes in Israel: Epidemiology, prevention and control. Int J Epidemiol. 1981;10:145-53.
- [Google Scholar]
- A contemporary analysis of road traffic crashes, fatalities and injuries in Trinidad and Tobago. Inj Control Saf Promot. 2003;10:21-7.
- [Google Scholar]
- Student drivers: A study of fatal motor vehicle crashes involving 16-year-old drivers. Ann Emerg Med. 2005;45:140-6.
- [Google Scholar]
- Epidemiologic characteristics of drivers, vehicles, pedestrians and road environments involved in road traffic injuries in rural Thailand. Southeast Asian J Trop Med Public Health. 1994;25:37-44.
- [Google Scholar]
- Deaths due to road traffic crashed in Hyderabad city in India: Need for strengthening surveillance. Natl Med J India. 2004;17:74-9.
- [Google Scholar]
- Pedestrian traffic injuries in Mexico: A country update. Inj Control Saf Promot. 2003;10:37-43.
- [Google Scholar]
- Trends in road traffic crashes and associated injury and fatality in the People's Republic of China, 1951-1999. Inj Control Saf Promot. 2003;10:83-7.
- [Google Scholar]
- Road traffic injuries in Kenya: Magnitude, causes and status of intervention. Inj Control Saf Promot. 2003;10:53-61.
- [Google Scholar]
- Evidence-based interventions for road traffic injuries in South Asia. J Coll Physicians Surg Pak. 2004;14:746-7.
- [Google Scholar]
- The profile of head injuries and traumatic brain injury deaths in Kashmir. J Trauma Manag Outcomes. 2008;21:5.
- [Google Scholar]
- Direct transport to tertiary trauma centers versus transfer from lower level facilities: Impact on mortality and morbidity among patients with major trauma. J Trauma. 1997;43:288-95.
- [Google Scholar]






